
Journal of Inorganic Materials ›› 2025, Vol. 40 ›› Issue (8): 921-932.DOI: 10.15541/jim20240541
• REVIEW • Previous Articles
Received:2024-12-27
Revised:2025-02-08
Published:2025-08-20
Online:2025-03-19
Contact:
LEI Bo, professor. E-mail: rayboo@xjtu.edu.cnAbout author:AI Minhui (2000-), female, Master candidate. E-mail: Aiminhui1023@stu.xjtu.edu.cn
Supported by:CLC Number:
AI Minhui, LEI Bo. Micro-nanoscale Bioactive Glass: Functionalized Design and Angiogenic Skin Regeneration[J]. Journal of Inorganic Materials, 2025, 40(8): 921-932.
| MNBG | Modulation of vascularization pattern | Ref. |
|---|---|---|
| Melt derived bioactive glass compositions | Degradation to release silicate ions to stimulate cell expressions of HIF-1α and VEGF | [ |
| BG/polydopamine electrostatically spun scaffolds | Promoting HUVECs expression of e-NOS, VEGF and angiogenic differentiation | [ |
| BG ointment with nanostructures | Promoting VEGF and FGF2 expression in the wound, resulting in a faster rate of granulation tissue formation and increased amounts of neovascularization and capillaries in the granulation | [ |
| Polyglycolic acid/BG composite scaffolds | Promoting VEGF release from fibroblasts, myocytes, hepatocytes, and neurons under hypoxic conditions | [ |
Table 1 Regulations of MNBG on angiogenesis during wound healing[19-22]
| MNBG | Modulation of vascularization pattern | Ref. |
|---|---|---|
| Melt derived bioactive glass compositions | Degradation to release silicate ions to stimulate cell expressions of HIF-1α and VEGF | [ |
| BG/polydopamine electrostatically spun scaffolds | Promoting HUVECs expression of e-NOS, VEGF and angiogenic differentiation | [ |
| BG ointment with nanostructures | Promoting VEGF and FGF2 expression in the wound, resulting in a faster rate of granulation tissue formation and increased amounts of neovascularization and capillaries in the granulation | [ |
| Polyglycolic acid/BG composite scaffolds | Promoting VEGF release from fibroblasts, myocytes, hepatocytes, and neurons under hypoxic conditions | [ |
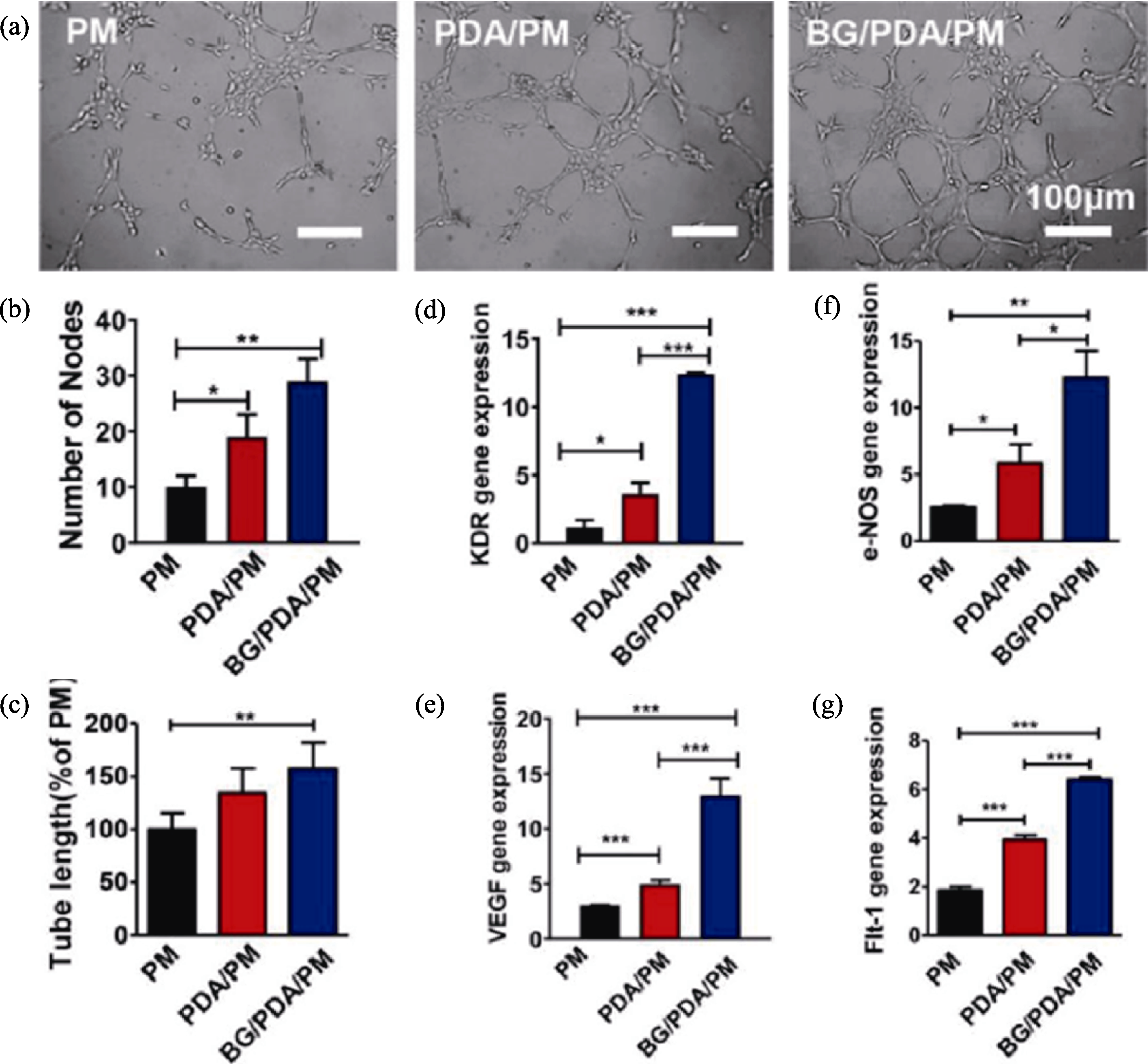
Fig. 3 Effect of different scaffolds (PM, PDA/PM and BG/PDA/PM) on angiogenesis in HUVECs[20] (a) Representative images for angiogenesis analysis; (b, c) Quantified node counts (b) and tube lengths (c); (d-g) Expressions of KDR (d), VEGF (e), e-NOS (f), and Flt-1 (g) in HUVECs cultured on composite scaffolds at 7 d (*: p<0.05; **: p<0.01; ***: p<0.001)
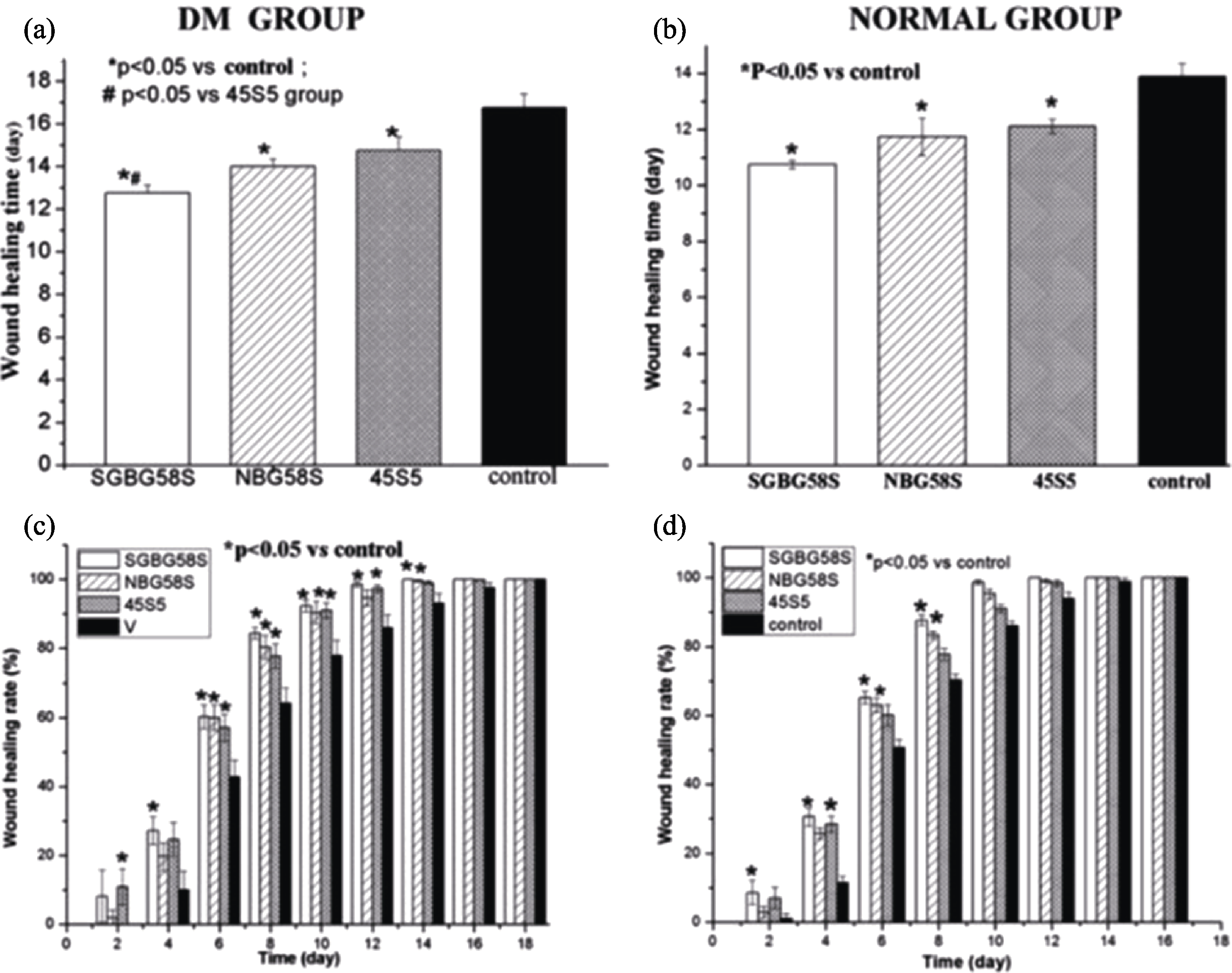
Fig. 4 Wound healing time and healing rate in rats[24] (a, b) Wound healing time in diabetic rats (a) and normal rats (b); (c, d) Wound healing rate in diabetic rats (c) normal rats (d) (n=8)
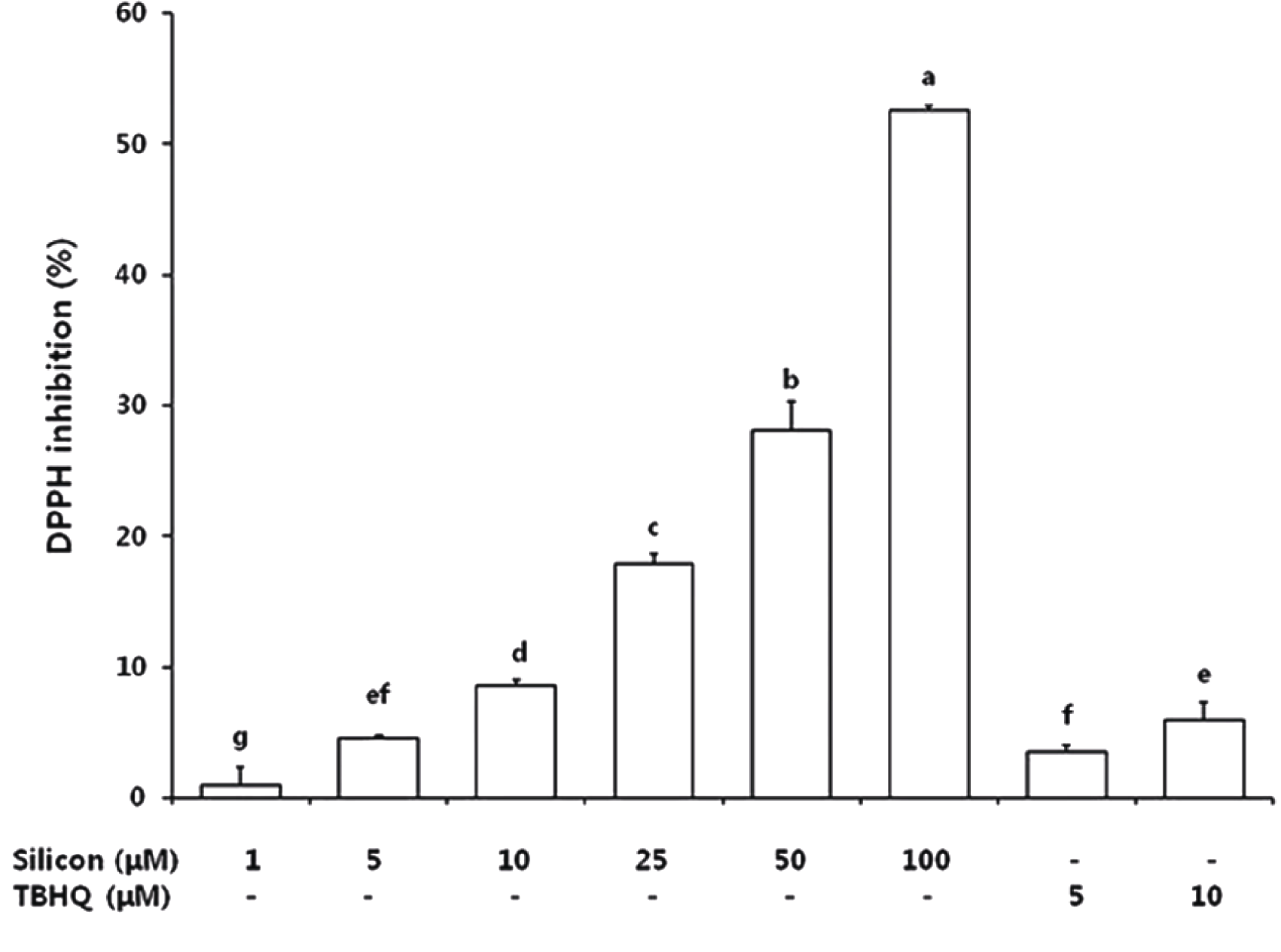
Fig. 5 DPPH free radical scavenging capacity of silicon and TBHQ treatments[55] TBHQ: tert-butyl hydroquinone; DPPH: 2,2-iphenyl-1-(2,4,6-trinitro- phenyl)hydrazyl
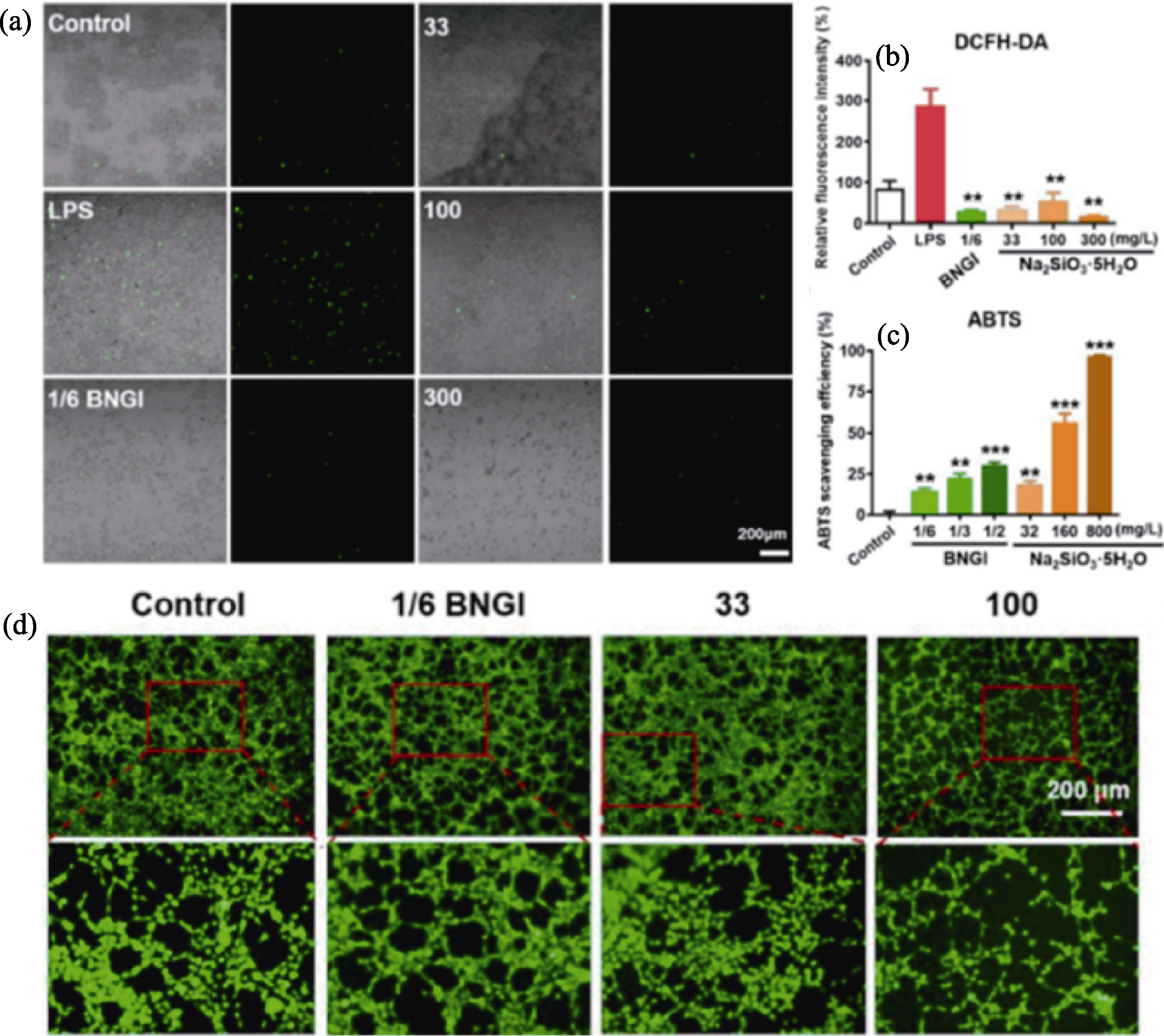
Fig. 6 Antioxidant effects of BNGI and Na2SiO3·5H2O[56] (a) ROS staining of macrophages stained with dichlorofluorescein diacetate (DCFH-DA) for 15 min to reflect ROS expression (green) after 1/6 BGNI treatment or 33, 100, and 300 mg/L Na2SiO3·5H2O addition for 2 d; (b) Quantitative analysis of relative fluorescence intensity measured using Image J (n=3, p<0.01 compared to LPS group); (c) Scavenging efficiency of 2,2'-biaminobis(3-ethylbenzothiazoline-6-sulfonic acid) (ABTS) of BNGI and Na2SiO3·5H2O in different concentrations based on the optical density values at 734 nm after 10 min incubation with ABTS reagent; (d) Fluorescent images of control, 1/6 BNGI or 33 and 100 mg/L Na2SiO3·5H2O pretreated for 2 d HUVECs after 8 h for angiogenic capacity analysis
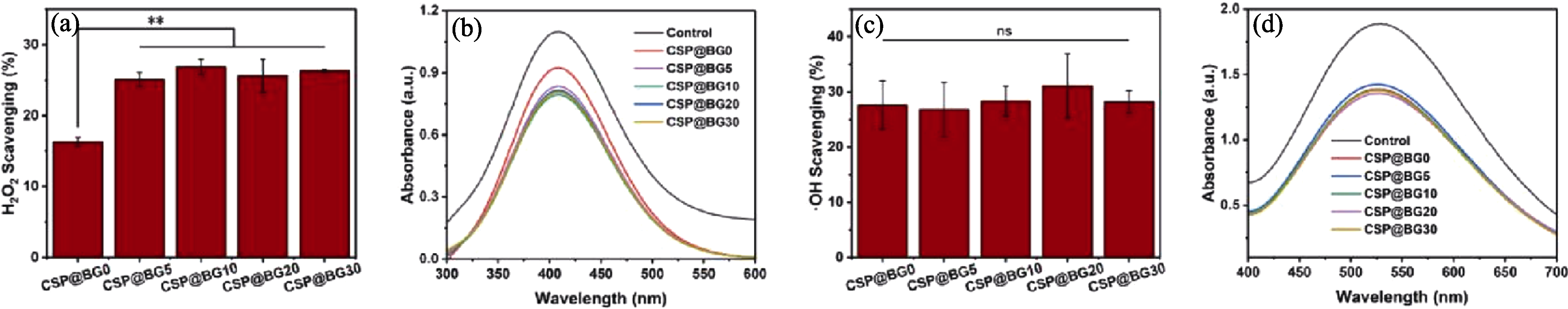
Fig. 7 Antioxidant activity of CSP@BG microspheres[59] (a) H2O2 scavenging percentage; (b) UV-Vis spectra of H2O2; (c) ·OH scavenging percentage; (d) UV-Vis spectra of OH. **: p<0.01
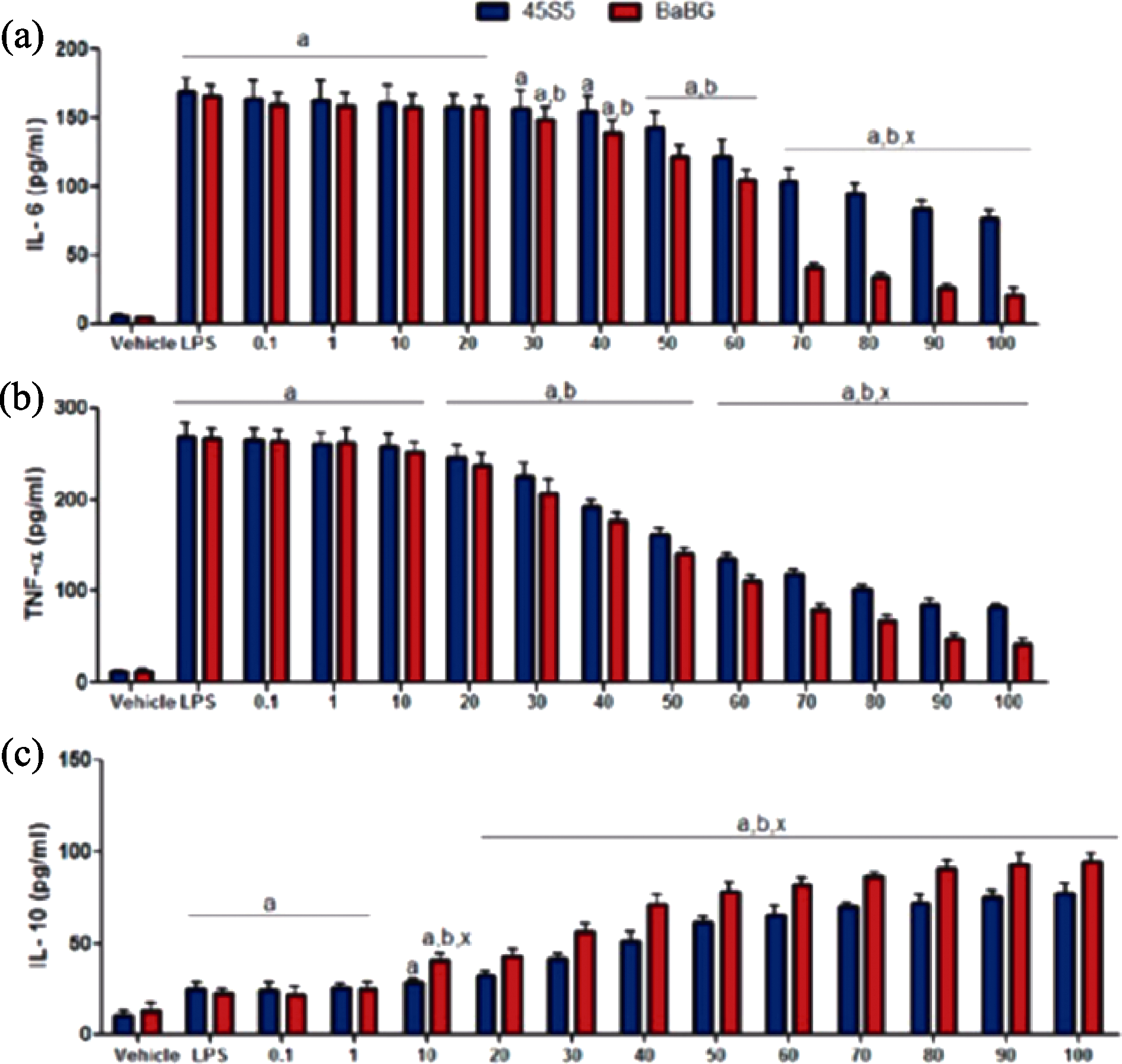
Fig. 8 Effect of BaBG and 45S5 on cytokine expression levels in C6 cells[65] IL-6: Interleukin-6; TNF-α: Tumor necrosis factor-α; IL-10: Interleukin-10
| Biological function | Material composition | Mode of action | Ref. |
|---|---|---|---|
| Pro-vascularization | PGA/BGN | Promotion of VEGF expression in fibroblasts | [ |
| BGN | Promotion of VEGF release from fibroblasts | [ | |
| MNBGN | Particle size in the range of 0.5-0.8 mm promoting VEGF expression | [ | |
| Immune cell modulation | BGN | Promoting chemotactic migration of neutrophils | [ |
| Zn-Mn- BGN | Mn and Si ions regulating M2 polarization in macrophages | [ | |
| Zn-BGN | Negative regulation of NF-κB signal | [ | |
| Cu-Zn-BBGN | Immunomodulation of DC viability | [ | |
| Antioxidation | BGN | Si scavenging activity on ROS | [ |
| Ce-MBGNs/CS | Scavenging activity on H2O2 | [ | |
| Anti-inflammatory | Ba-BGN | Elevation of anti-inflammatory cytokine IL-10 | [ |
| Ce-MBGNs | Decreasing expression of inflammatory factors TNF-α and IL-1β | [ | |
| Antimicrobial | BGN | High pH and alkaline ions enhancing antimicrobial activity | [ |
| BGN | 58S and 63S for broad-spectrum antibacterial | [ | |
| Ce-MBGNs | Mesoporous structure promoting antimicrobial activity | [ | |
| Cu-MBGNs | Broad-spectrum antimicrobial effect of Cu | [ |
Table 2 Mechanism of MNBG for vascularized skin repair
| Biological function | Material composition | Mode of action | Ref. |
|---|---|---|---|
| Pro-vascularization | PGA/BGN | Promotion of VEGF expression in fibroblasts | [ |
| BGN | Promotion of VEGF release from fibroblasts | [ | |
| MNBGN | Particle size in the range of 0.5-0.8 mm promoting VEGF expression | [ | |
| Immune cell modulation | BGN | Promoting chemotactic migration of neutrophils | [ |
| Zn-Mn- BGN | Mn and Si ions regulating M2 polarization in macrophages | [ | |
| Zn-BGN | Negative regulation of NF-κB signal | [ | |
| Cu-Zn-BBGN | Immunomodulation of DC viability | [ | |
| Antioxidation | BGN | Si scavenging activity on ROS | [ |
| Ce-MBGNs/CS | Scavenging activity on H2O2 | [ | |
| Anti-inflammatory | Ba-BGN | Elevation of anti-inflammatory cytokine IL-10 | [ |
| Ce-MBGNs | Decreasing expression of inflammatory factors TNF-α and IL-1β | [ | |
| Antimicrobial | BGN | High pH and alkaline ions enhancing antimicrobial activity | [ |
| BGN | 58S and 63S for broad-spectrum antibacterial | [ | |
| Ce-MBGNs | Mesoporous structure promoting antimicrobial activity | [ | |
| Cu-MBGNs | Broad-spectrum antimicrobial effect of Cu | [ |
| [1] | ZHENG K, TORRE E, BARI A, et al. Antioxidant mesoporous Ce-doped bioactive glass nanoparticles with anti-inflammatory and pro-osteogenic activities. Materials Today Bio, 2020, 5: 100041. |
| [2] | SKALLEVOLD H E, ROKAYA D, KHURSHID Z, et al. Bioactive glass applications in dentistry. International Journal of Materials Science, 2019, 20: 5960. |
| [3] |
MAJUMDAR S, GUPTA S, KRISHNAMURTHY S. Multifarious applications of bioactive glasses in soft tissue engineering. Biomaterials Science, 2021, 9: 8111.
DOI PMID |
| [4] | HONG Z, REIS R L, MANO J F. Preparation and in vitro characterization of scaffolds of poly(L-lactic acid) containing bioactive glass ceramic nanoparticles. Acta Biomaterialia, 2008, 4: 1297. |
| [5] |
REZWAN K, CHEN Q Z, BLAKER J J, et al. Biodegradable and bioactive porous polymer/inorganic composite scaffolds for bone tissue engineering. Biomaterials, 2006, 27: 3413.
DOI PMID |
| [6] | HU Q, JIANG W, LI Y, et al. The effects of morphology on physicochemical properties, bioactivity and biocompatibility of micro-/nano-bioactive glasses. Advanced Powder Technology, 2018, 29: 1812. |
| [7] |
HUANG X L, TENG X, CHEN D, et al. The effect of the shape of mesoporous silica nanoparticles on cellular uptake and cell function. Biomaterials, 2010, 31: 438.
DOI PMID |
| [8] | LI H, LI D, WANG X, et al. Progress in biomaterials-enhanced vascularization by modulating physical properties. ACS Biomaterials Science & Engineering, 2025, 11: 33. |
| [9] |
ALOUI C, PRIGENT A, SUT C, et al. The signaling role of CD40 ligand in platelet biology and in platelet component transfusion. International Journal of Molecular Sciences, 2014, 15(12): 22342.
DOI PMID |
| [10] |
CHAKRABARTI S, RIZVI M, MORIN K, et al. The role of CD40L and VEGF in the modulation of angiogenesis and inflammation. Vascular Pharmacology, 2010, 53: 130.
DOI PMID |
| [11] |
PHILLIPSON M, KUBES P. The healing power of neutrophils. Trends in Immunology, 2019, 40: 635.
DOI PMID |
| [12] |
ZHENG K, NIU W, LEI B, et al. Immunomodulatory bioactive glasses for tissue regeneration. Acta Biomaterialia, 2021, 133: 168.
DOI PMID |
| [13] | MUGHAL A, GILLANI S M H, AHMED S, et al. 3D-printed polyether-ether ketone/carboxymethyl cellulose scaffolds coated with Zn-Mn doped mesoporous bioactive glass nanoparticles. Journal of the Mechanical Behavior of Biomedical Materials, 2024, 156: 106581. |
| [14] | POLO-MONTALVO A, CASARRUBIOS L, SERRANO M C, et al. Effective actions of ion release from mesoporous bioactive glass and macrophage mediators on the differentiation of osteoprogenitor and endothelial progenitor cells. Pharmaceutics, 2021, 13(8):1152. |
| [15] | VARMETTE E A, NOWALK J R, FLICK L M, et al. Abrogation of the inflammatory response in LPS-stimulated RAW 264.7 murine macrophages by Zn- and Cu-doped bioactive Sol-Gel glasses. Journal of Biomedical Materials Research Part A, 2009, 90A: 317. |
| [16] |
WANG L, WEI X, WANG Y. Promoting angiogenesis using immune cells for tissue-engineered vascular grafts. Annals of Biomedical Engineering, 2023, 51: 660.
DOI PMID |
| [17] | SOZZANI S, RUSNATI M, RIBOLDI E, et al. Dendritic cell- endothelial cell cross-talk in angiogenesis. Trends in Immunology, 2007, 28: 385. |
| [18] | ZARUBOVA J, HASANI-SADRABADI M M, ARDEHALI R, et al. Immunoengineering strategies to enhance vascularization and tissue regeneration. Advanced Drug Delivery Reviews, 2022, 184: 114233. |
| [19] |
SOLANKI A K, LALI F V, AUTEFAGE H, et al. Bioactive glasses and electrospun composites that release cobalt to stimulate the HIF pathway for wound healing applications. Biomaterials Research, 2021, 25: 1.
DOI PMID |
| [20] |
JIANG Y, LI Y, LI J, et al. A mussel-inspired extracellular matrix-mimicking composite scaffold for diabetic wound healing. ACS Applied Bio Materials, 2020, 3: 4052.
DOI PMID |
| [21] |
LI H, CHANG J. Stimulation of proangiogenesis by calcium silicate bioactive ceramic. Acta Biomaterialia, 2013, 9: 5379.
DOI PMID |
| [22] |
DAY R M, BOCCACCINI A R, SHUREY S, et al. Assessment of polyglycolic acid mesh and bioactive glass for soft-tissue engineering scaffolds. Biomaterials, 2004, 25: 5857.
PMID |
| [23] |
LI R, CLARK A E, HENCH L L. An investigation of bioactive glass powders by Sol-Gel processing. Journal of Applied Biomaterials, 1991, 2: 231.
PMID |
| [24] | LIN C, MAO C, ZHANG J J, et al. Healing effect of bioactive glass ointment on full-thickness skin wounds. Biomedical Materials, 2012, 7: 045017. |
| [25] | LU Y, YANG Y, XIAO L, et al. Autocrine and paracrine effects of vascular endothelial cells promote cutaneous wound healing. BioMed Research International, 2021, 10: 6695663. |
| [26] | JIN L, LONG Y, ZHANG Q, et al. MiRNAs regulate cell communication in osteogenesis-angiogenesis coupling during bone regeneration. Molecular Biology Reports, 2023, 50: 8715. |
| [27] |
HOPPE A, GÜLDAL N S, BOCCACCINI A R. A review of the biological response to ionic dissolution products from bioactive glasses and glass-ceramics. Biomaterials, 2011, 32: 2757.
DOI PMID |
| [28] |
WU C T, ZHOU Y H, XU M C, et al. Copper-containing mesoporous bioactive glass scaffolds with multifunctional properties of angiogenesis capacity, osteostimulation and antibacterial activity. Biomaterials, 2013, 34: 422.
DOI PMID |
| [29] |
WU C T, ZHOU Y H, FAN W, et al. Hypoxia-mimicking mesoporous bioactive glass scaffolds with controllable cobalt ion release for bone tissue engineering. Biomaterials, 2012, 33: 2076.
DOI PMID |
| [30] |
PATEL U, MOSS R M, HOSSAIN K M Z, et al. Structural and physico-chemical analysis of calcium/strontium substituted, near-invert phosphate based glasses for biomedical applications. Acta Biomaterialia, 2017, 60: 109.
DOI PMID |
| [31] | BOCCARDI E, CIRALDO F E, BOCCACCINI A R. Bioactive glass-ceramic scaffolds: processing and properties. MRS Bulletin, 2017, 42: 226. |
| [32] | LEU A, LEACH J K. Proangiogenic potential of a collagen/ bioactive glass substrate. Pharmaceutical Research, 2008, 25: 1222. |
| [33] | LIN Y, XIAO W, LIU X, et al. Long-term bone regeneration, mineralization and angiogenesis in rat calvarial defects implanted with strong porous bioactive glass (13-93) scaffolds. Journal of Non-Crystalline Solids, 2016, 432: 120. |
| [34] | LI Y, CHEN L, CHEN X, et al. High phosphate content in bioactive glasses promotes osteogenesis in vitro and in vivo. Dental Materials, 2021, 37: 272. |
| [35] | GERHARDT L C, WIDDOWS K L, EROL M M, et al. The pro-angiogenic properties of multi-functional bioactive glass composite scaffolds. Biomaterials, 2011, 32: 4096. |
| [36] |
DETSCH R, STOOR P, GRÜNEWALD A, et al. Increase in VEGF secretion from human fibroblast cells by bioactive glass S53P4 to stimulate angiogenesis in bone. Journal of Biomedical Materials Research Part A, 2014, 102: 4055.
DOI PMID |
| [37] | ZHU Y, MA Z, KONG L, et al. Modulation of macrophages by bioactive glass/sodium alginate hydrogel is crucial in skin regeneration enhancement. Biomaterials, 2020, 256: 120216. |
| [38] | SINGER B D, CHANDEL N S. Immunometabolism of pro-repair cells. The Journal of Clinical Investigation, 2019, 129: 2597. |
| [39] | MARTIN P, LEIBOVICH S J. Inflammatory cells during wound repair: the good, the bad and the ugly. Trends Cell Biology, 2005, 15: 599. |
| [40] |
AHMADI A R, CHICCO M, HUANG J, et al. Stem cells in burn wound healing: a systematic review of the literature. Burns, 2019, 45: 1014.
DOI PMID |
| [41] | WANG S, YANG J, ZHAO G, et al. Current applications of platelet gels in wound healing: a review. Wound Repair and Regeneration, 2021, 29: 370. |
| [42] |
SUMMERS C, RANKIN S M, CONDLIFFE A M, et al. Neutrophil kinetics in health and disease. Trends in Immunology, 2010, 31: 318.
DOI PMID |
| [43] |
BURN G L, FOTI A, MARSMAN G, et al. The neutrophil. Immunity, 2021, 54: 1377.
DOI PMID |
| [44] | BASHIR S, SHARMA Y, ELAHI A, et al. Macrophage polarization: the link between inflammation and related diseases. Inflammatory Research, 2016, 65: 1. |
| [45] | YUNNA C, MENGRU H, LEI W, et al. Macrophage M1/M2 polarization. European Journal of Pharmacology, 2020, 877: 173090. |
| [46] |
SPILLER K L, ANFANG R R, SPILLER K J, et al. The role of macrophage phenotype in vascularization of tissue engineering scaffolds. Biomaterials, 2014, 35: 4477.
DOI PMID |
| [47] |
GRANEY P L, BEN-SHAUL S, LANDAU S, et al. Macrophages of diverse phenotypes drive vascularization of engineered tissues. Science Advances, 2020, 6: 6391.
DOI PMID |
| [48] |
KREIMENDAHL F, MARQUARDT Y, APEL C, et al. Macrophages significantly enhance wound healing in a vascularized skin model. Journal of Biomedical Materials Research Part A, 2019, 107: 1340.
DOI PMID |
| [49] | YANG M, MA C, LIU S, et al. HIF-dependent induction of adenosine receptor A2b skews human dendritic cells to a Th2-stimulating phenotype under hypoxia. Immunology & Cell Biology, 2010, 88: 165. |
| [50] | BAI W K, ZHANG W, HU B. Vascular endothelial growth factor suppresses dendritic cells function of human prostate cancer. OncoTargets and Therapy, 2018, 11: 1267. |
| [51] | SCHUHLADEN K, STICH L, SCHMIDT J, et al. Cu, Zn doped borate bioactive glasses: antibacterial efficacy and dose-dependent in vitro modulation of murine dendritic cells. Biomaterials Science, 2020, 8: 2143. |
| [52] |
KWEE B J, BUDINA E, NAJIBI A J, et al. CD4 T-cells regulate angiogenesis and myogenesis. Biomaterials, 2018, 178: 109.
DOI PMID |
| [53] |
RAUSCHENBERGER T, SCHMITT V, AZEEM M, et al. T cells control chemokine secretion by keratinocytes. Frontiers in Immunology, 2019, 10: 1917.
DOI PMID |
| [54] | GROME H N, BARNETT L, HAGAR C C, et al. Association of T cell and macrophage activation with arterial vascular health in HIV. AIDS Research and Human Retroviruses, 2016, 33: 181. |
| [55] | KIM E J, BU S Y, SUNG M K, et al. Analysis of antioxidant and anti-inflammatory activity of silicon in murine macrophages. Biological Trace Element Research, 2013, 156: 329. |
| [56] | LIU W, CHEN M, LUO M, et al. Bioactive glass ions hydrogels with antiinflammation antioxidant capacity for treating inflammation- related diseases. Materials & Design, 2023, 227: 111669. |
| [57] |
NIELSEN F H. A novel silicon complex is as effective as sodium metasilicate in enhancing the collagen-induced inflammatory response of silicon-deprived rats. Journal of Trace Elements in Medicine and Biology, 2008, 22: 39.
DOI PMID |
| [58] |
BIRBEN E, SAHINER U M, SACKESEN C, et al. Oxidative stress and antioxidant defense. World Allergy Organization Journal, 2012, 5: 9.
DOI PMID |
| [59] | XU W, QIN Z, XU R, et al. Injectable, pro-osteogenic and antioxidant composite microspheres composed of cerium- containing mesoporous bioactive glass and chitosan for bone regeneration applications. Ceramics International, 2023, 49: 25757. |
| [60] | ZHU Y, ZHANG X, CHANG G, et al. Bioactive glass in tissue regeneration: unveiling recent advances in regenerative strategies and applications. Advanced Materials, 2025, 37: 2312964. |
| [61] |
LOSI P, BRIGANTI E, ERRICO C, et al. Fibrin-based scaffold incorporating VEGF- and bFGF-loaded nanoparticles stimulates wound healing in diabetic mice. Acta Biomaterialia, 2013, 9: 7814.
DOI PMID |
| [62] | FRANK S, HÜBNER G, BREIER G, et al. Regulation of vascular endothelial growth factor expression in cultured keratinocytes. Journal of Biological Chemistry, 1995, 270: 12607. |
| [63] | EL-FIQI A, ALLAM R, KIM H W. Antioxidant cerium ions- containing mesoporous bioactive glass ultrasmall nanoparticles: structural, physico-chemical, catalase-mimic and biological properties. Colloids and Surfaces B: Biointerfaces, 2021, 206: 111932. |
| [64] | EBERSBERGER A, SCHAIBLE H G. Do cytokines play a role in the transition from acute to chronic musculoskeletal pain. Pharmacological Research, 2025, 212: 107585. |
| [65] | MAJUMDAR S, HIRA S K, TRIPATHI H, et al. Synthesis and characterization of barium-doped bioactive glass with potential anti- inflammatory activity. Ceramics International, 2021, 47: 7143. |
| [66] |
JUNG H, LEE H, KIM D, et al. Differential regional vulnerability of the brain to mild neuroinflammation induced by systemic LPS treatment in mice. Journal of Inflammation Research, 2022, 15: 3053.
DOI PMID |
| [67] | DUAN Y, ZHENG K, HU W, et al. Anti-inflammatory cerium- containing nano-scaled mesoporous bioactive glass for promoting regenerative capability of dental pulp cells. International Endodontic Journal, 2024, 57: 727. |
| [68] |
KANG Y, LIU K, CHEN Z, et al. Healing with precision: a multi-functional hydrogel-bioactive glass dressing boosts infected wound recovery and enhances neurogenesis in the wound bed. Journal of Controlled Release, 2024, 370: 210.
DOI PMID |
| [69] | ZHANG D, LEPPÄRANTA O, MUNUKKA E, et al. Antibacterial effects and dissolution behavior of six bioactive glasses. Journal of Biomedical Materials Research Part A, 2010, 93A: 475. |
| [70] | ZEHNDER M, WALTIMO T, SENER B, et al. Dentin enhances the effectiveness of bioactive glass S53P4 against a strain of Enterococcus faecalis. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontoligy, 2006, 101: 530. |
| [71] | MORTAZAVI V, NAHRKHALAJI M M, FATHI M H, et al. Antibacterial effects of Sol-Gel-derived bioactive glass nanoparticle on aerobic bacteria. Journal of Biomedical Materials Research Part A, 2010, 94A: 160. |
| [72] | HU G, XIAO L, TONG P, et al. Antibacterial hemostatic dressings with nanoporous bioglass containing silver. International Journal Nanomedicine, 2012; 7: 2613. |
| [73] | HAN X, CHEN Y, JIANG Q, et al. Novel bioactive glass-modified hybrid composite resin: mechanical properties, biocompatibility, and antibacterial and remineralizing activity. Frontiers in Bioengineering and Biotechnology, 2021, 9: 661734. |
| [74] | ÖZARSLAN A C. Preparation of biosilica glass-based porous scaffolds using various elements (Mg-Zn, Mg-Cu, and Sr-Cu) as bioactive glass co-dopants: in vitro bioactivity and biocompatibility behaviors. Journal of Materials Research, 2023, 38: 3874. |
| [75] | KURTULDU F, KAŇKOVÁ H, BELTRÁN A M, et al. Anti- inflammatory and antibacterial activities of cerium-containing mesoporous bioactive glass nanoparticles for drug-free biomedical applications. Materials Today Bio, 2021, 12: 100150. |
| [76] | POP O L, MESAROS A, VODNAR D C, et al. Cerium oxide nanoparticles and their efficient antibacterial application in vitro against gram-positive and gram-negative pathogens. Nanomaterials, 2020, 10: 1614. |
| [77] | MUTLU N, KURTULDU F, UNALAN I, et al. Effect of Zn and Ga doping on bioactivity, degradation, and antibacterial properties of borate 1393-B3 bioactive glass. Ceramics International, 2022, 48: 16404. |
| [78] | LI T, WANG Y, LEI B. Photothermal-antibacterial bioactive noncrystalline nanosystem promotes infected wound tissue regeneration through thermo-ions activation. Chemical Engineering Journal, 2024, 491: 151799. |
| [1] | YU Shengyang, SU Haijun, JIANG Hao, YU Minghui, YAO Jiatong, YANG Peixin. A Review of Pore Defects in Ultra-high Temperature Oxide Ceramics by Laser Additive Manufacturing: Formation and Suppression [J]. Journal of Inorganic Materials, 2025, 40(9): 944-956. |
| [2] | LIU Jiangping, GUAN Xin, TANG Zhenjie, ZHU Wenjie, LUO Yongming. Research Progress on Catalytic Oxidation of Nitrogen-containing Volatile Organic Compounds [J]. Journal of Inorganic Materials, 2025, 40(9): 933-943. |
| [3] | XIAO Xiaolin, WANG Yuxiang, GU Peiyang, ZHU Zhenrong, SUN Yong. Advances in Regulation of Damaged Skin Regeneration by Two-dimensional Inorganic Materials [J]. Journal of Inorganic Materials, 2025, 40(8): 860-870. |
| [4] | MA Jingge, WU Chengtie. Application of Inorganic Bioceramics in Promoting Hair Follicle Regeneration and Hair Growth [J]. Journal of Inorganic Materials, 2025, 40(8): 901-910. |
| [5] | ZHANG Hongjian, ZHAO Ziyi, WU Chengtie. Inorganic Biomaterials on Regulating Neural Cell Function and Innervated Tissue Regeneration: A Review [J]. Journal of Inorganic Materials, 2025, 40(8): 849-859. |
| [6] | WANG Yutong, CHANG Jiang, XU He, WU Chengtie. Advances in Silicate Bioceramic/Bioglass for Wound Healing: Effects, Mechanisms and Application Ways [J]. Journal of Inorganic Materials, 2025, 40(8): 911-920. |
| [7] | MA Wenping, HAN Yahui, WU Chengtie, LÜ Hongxu. Application of Inorganic Bioactive Materials in Organoid Research [J]. Journal of Inorganic Materials, 2025, 40(8): 888-900. |
| [8] | LUO Xiaomin, QIAO Zhilong, LIU Ying, YANG Chen, CHANG Jiang. Inorganic Bioactive Materials Regulating Myocardial Regeneration [J]. Journal of Inorganic Materials, 2025, 40(8): 871-887. |
| [9] | ZHU Wenjie, TANG Lu, LU Jichang, LIU Jiangping, LUO Yongming. Research Progress on Catalytic Oxidation of Volatile Organic Compounds by Perovskite Oxides [J]. Journal of Inorganic Materials, 2025, 40(7): 735-746. |
| [10] | HU Zhichao, YANG Hongyu, YANG Hongcheng, SUN Chengli, YANG Jun, LI Enzhu. Usage of the P-V-L Bond Theory in Regulating Properties of Microwave Dielectric Ceramics [J]. Journal of Inorganic Materials, 2025, 40(6): 609-626. |
| [11] | WU Qiong, SHEN Binglin, ZHANG Maohua, YAO Fangzhou, XING Zhipeng, WANG Ke. Research Progress on Lead-based Textured Piezoelectric Ceramics [J]. Journal of Inorganic Materials, 2025, 40(6): 563-574. |
| [12] | ZHANG Bihui, LIU Xiaoqiang, CHEN Xiangming. Recent Progress of Hybrid Improper Ferroelectrics with Ruddlesden-Popper Structure [J]. Journal of Inorganic Materials, 2025, 40(6): 587-608. |
| [13] | WU Jie, YANG Shuai, WANG Mingwen, LI Jinglei, LI Chunchun, LI Fei. Textured PT-based Piezoelectric Ceramics: Development, Status and Challenge [J]. Journal of Inorganic Materials, 2025, 40(6): 575-586. |
| [14] | JIANG Kun, LI Letian, ZHENG Mupeng, HU Yongming, PAN Qinxue, WU Chaofeng, WANG Ke. Research Progress on Low-temperature Sintering of PZT Ceramics [J]. Journal of Inorganic Materials, 2025, 40(6): 627-638. |
| [15] | TIAN Ruizhi, LAN Zhengyi, YIN Jie, HAO Nanjing, CHEN Hangrong, MA Ming. Microfluidic Technology Based Synthesis of Inorganic Nano-biomaterials: Principles and Progress [J]. Journal of Inorganic Materials, 2025, 40(4): 337-347. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
