无机材料学报 ›› 2025, Vol. 40 ›› Issue (8): 921-932.DOI: 10.15541/jim20240541 CSTR: 32189.14.jim20240541
• 综述 • 上一篇
收稿日期:2024-12-27
修回日期:2025-02-08
出版日期:2025-08-20
网络出版日期:2025-03-19
通讯作者:
雷 波, 教授. E-mail: rayboo@xjtu.edu.cn作者简介:艾敏慧(2000-), 女, 硕士研究生. E-mail: Aiminhui1023@stu.xjtu.edu.cn
基金资助:Received:2024-12-27
Revised:2025-02-08
Published:2025-08-20
Online:2025-03-19
Contact:
LEI Bo, professor. E-mail: rayboo@xjtu.edu.cnAbout author:AI Minhui (2000-), female, Master candidate. E-mail: Aiminhui1023@stu.xjtu.edu.cn
Supported by:摘要:
生物活性玻璃(BG)材料是一类重要的非晶态无机医用材料, 在硬组织修复领域临床应用多年, 表现出独特的组织修复活性。近年研究发现, BG在促进软组织修复方面也表现出有效的修复活性, 具有重要的应用价值。与传统BG相比, 微纳米生物活性玻璃(MNBG)具有独特的微纳米结构, 不仅保留了传统BG优良的化学组成, 而且具有更大的比表面积和更高的反应活性, 在促进血管化皮肤修复再生方面表现出重要的应用潜力。本文重点讨论了MNBG在调控血管化及皮肤再生方面的研究进展, 主要包括MNBG促进血管化的能力, 调控免疫细胞的功能, 以及抗氧化、抗炎和抗菌性能, 这些特性使得MNBG能够有效刺激血管形成, 同时降低炎症反应, 抑制细菌感染, 从而促进伤口愈合和组织修复。进一步总结了MNBG在皮肤创面血管化和修复方面的重要研究进展, 并对MNBG目前皮肤创面修复应用中存在的问题和未来的研究方向提出了相应的建议, 以期推动MNBG在皮肤修复领域中的应用转化。
中图分类号:
艾敏慧, 雷波. 微纳米生物活性玻璃: 功能化设计与血管化皮肤再生[J]. 无机材料学报, 2025, 40(8): 921-932.
AI Minhui, LEI Bo. Micro-nanoscale Bioactive Glass: Functionalized Design and Angiogenic Skin Regeneration[J]. Journal of Inorganic Materials, 2025, 40(8): 921-932.
| MNBG | Modulation of vascularization pattern | Ref. |
|---|---|---|
| Melt derived bioactive glass compositions | Degradation to release silicate ions to stimulate cell expressions of HIF-1α and VEGF | [ |
| BG/polydopamine electrostatically spun scaffolds | Promoting HUVECs expression of e-NOS, VEGF and angiogenic differentiation | [ |
| BG ointment with nanostructures | Promoting VEGF and FGF2 expression in the wound, resulting in a faster rate of granulation tissue formation and increased amounts of neovascularization and capillaries in the granulation | [ |
| Polyglycolic acid/BG composite scaffolds | Promoting VEGF release from fibroblasts, myocytes, hepatocytes, and neurons under hypoxic conditions | [ |
表1 MNBG在创面修复过程中对血管化的调控[19-22]
Table 1 Regulations of MNBG on angiogenesis during wound healing[19-22]
| MNBG | Modulation of vascularization pattern | Ref. |
|---|---|---|
| Melt derived bioactive glass compositions | Degradation to release silicate ions to stimulate cell expressions of HIF-1α and VEGF | [ |
| BG/polydopamine electrostatically spun scaffolds | Promoting HUVECs expression of e-NOS, VEGF and angiogenic differentiation | [ |
| BG ointment with nanostructures | Promoting VEGF and FGF2 expression in the wound, resulting in a faster rate of granulation tissue formation and increased amounts of neovascularization and capillaries in the granulation | [ |
| Polyglycolic acid/BG composite scaffolds | Promoting VEGF release from fibroblasts, myocytes, hepatocytes, and neurons under hypoxic conditions | [ |
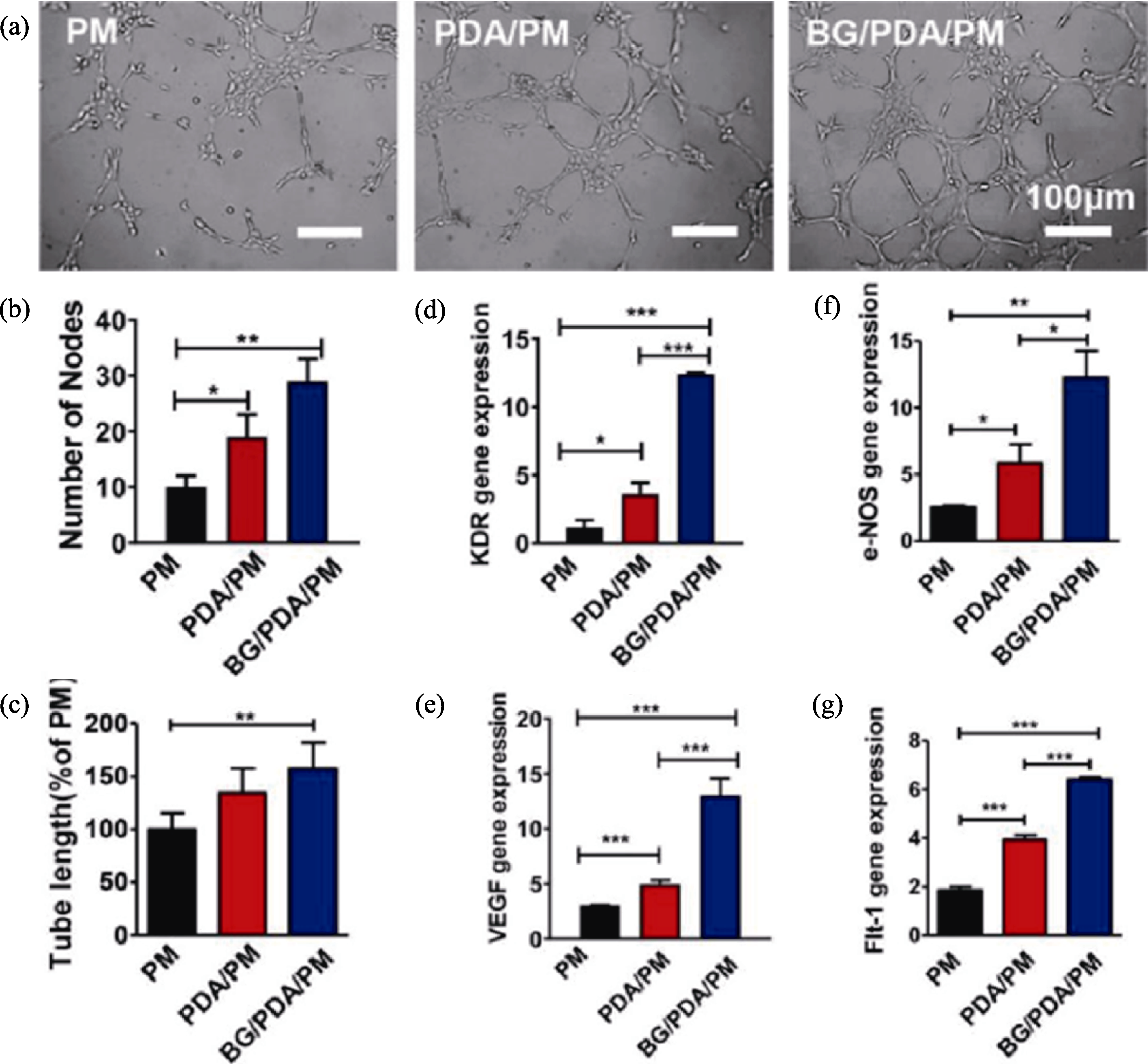
图3 不同支架(PM、PDA/PM和BG/PDA/PM)对HUVECs成血管的影响[20]
Fig. 3 Effect of different scaffolds (PM, PDA/PM and BG/PDA/PM) on angiogenesis in HUVECs[20] (a) Representative images for angiogenesis analysis; (b, c) Quantified node counts (b) and tube lengths (c); (d-g) Expressions of KDR (d), VEGF (e), e-NOS (f), and Flt-1 (g) in HUVECs cultured on composite scaffolds at 7 d (*: p<0.05; **: p<0.01; ***: p<0.001)
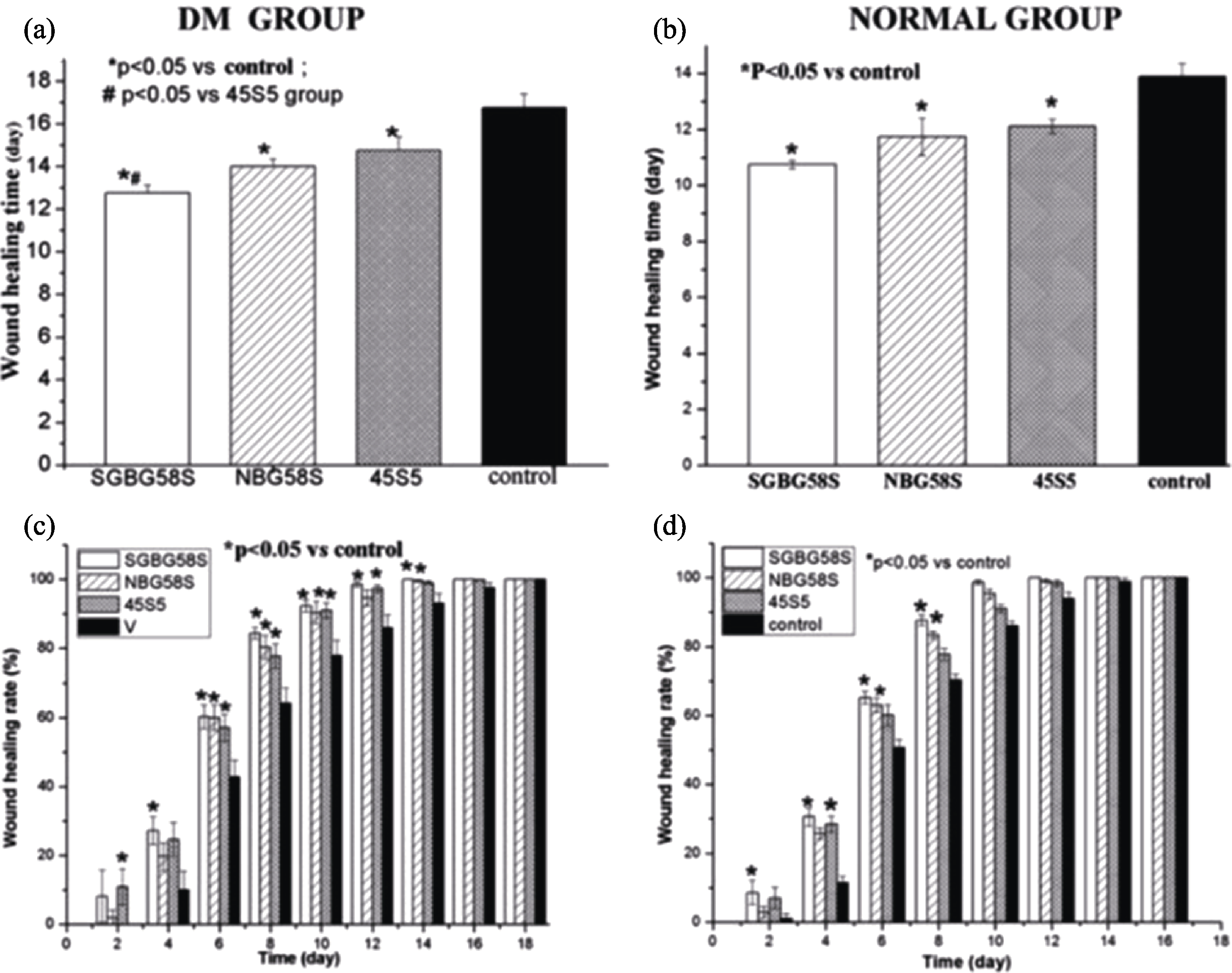
图4 大鼠的伤口愈合时间和愈合率[24]
Fig. 4 Wound healing time and healing rate in rats[24] (a, b) Wound healing time in diabetic rats (a) and normal rats (b); (c, d) Wound healing rate in diabetic rats (c) normal rats (d) (n=8)
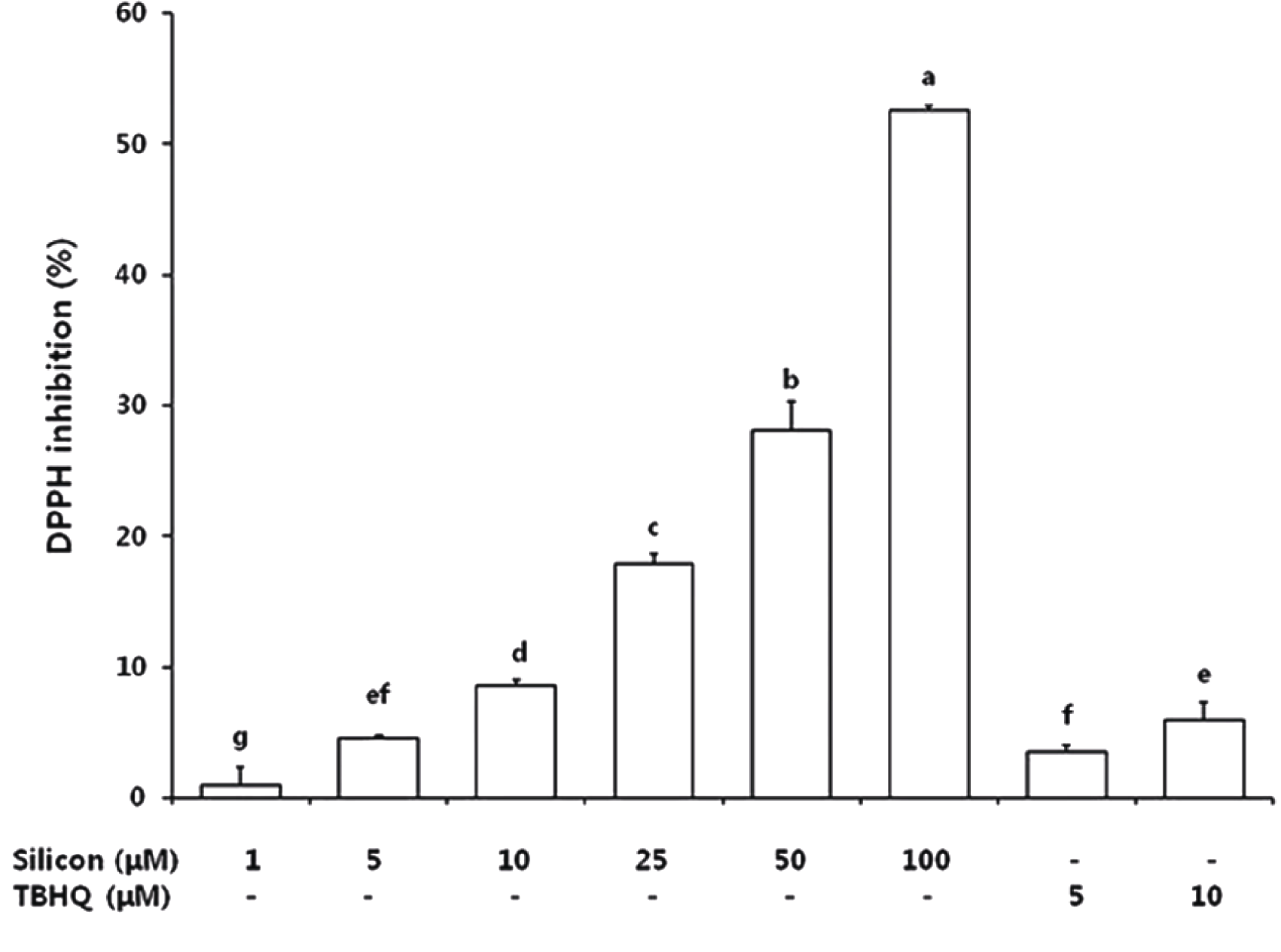
图5 Si和TBHQ处理的DPPH自由基清除能力[55]
Fig. 5 DPPH free radical scavenging capacity of silicon and TBHQ treatments[55] TBHQ: tert-butyl hydroquinone; DPPH: 2,2-iphenyl-1-(2,4,6-trinitro- phenyl)hydrazyl
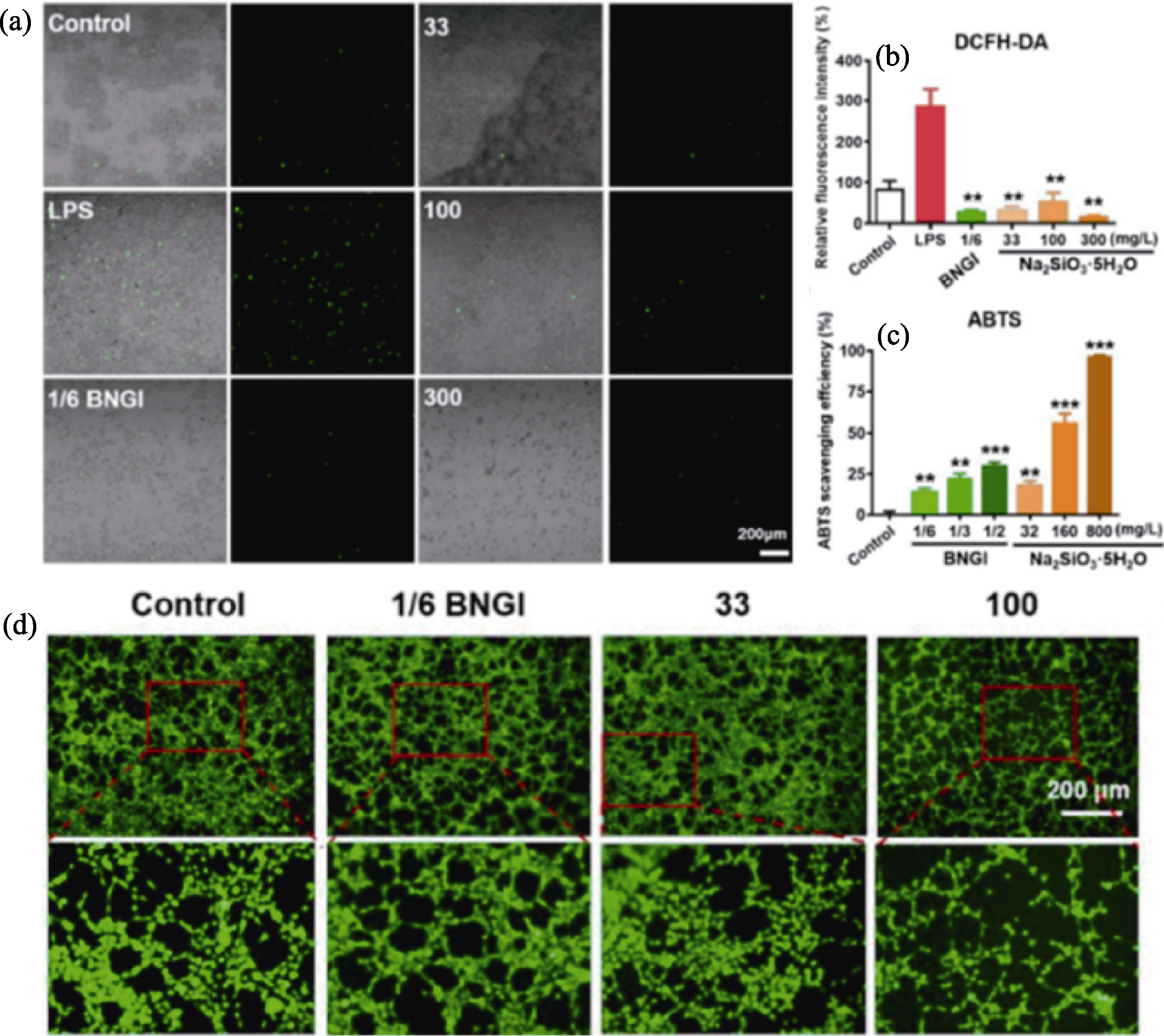
图6 BNGI和Na2SiO3·5H2O的抗氧化作用[56]
Fig. 6 Antioxidant effects of BNGI and Na2SiO3·5H2O[56] (a) ROS staining of macrophages stained with dichlorofluorescein diacetate (DCFH-DA) for 15 min to reflect ROS expression (green) after 1/6 BGNI treatment or 33, 100, and 300 mg/L Na2SiO3·5H2O addition for 2 d; (b) Quantitative analysis of relative fluorescence intensity measured using Image J (n=3, p<0.01 compared to LPS group); (c) Scavenging efficiency of 2,2'-biaminobis(3-ethylbenzothiazoline-6-sulfonic acid) (ABTS) of BNGI and Na2SiO3·5H2O in different concentrations based on the optical density values at 734 nm after 10 min incubation with ABTS reagent; (d) Fluorescent images of control, 1/6 BNGI or 33 and 100 mg/L Na2SiO3·5H2O pretreated for 2 d HUVECs after 8 h for angiogenic capacity analysis
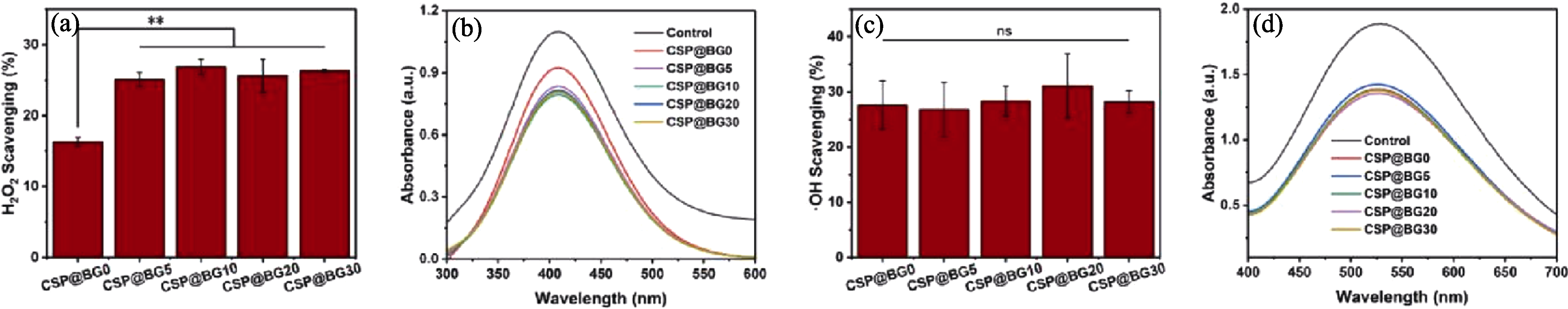
图7 CSP@BG微球的抗氧化活性[59]
Fig. 7 Antioxidant activity of CSP@BG microspheres[59] (a) H2O2 scavenging percentage; (b) UV-Vis spectra of H2O2; (c) ·OH scavenging percentage; (d) UV-Vis spectra of OH. **: p<0.01
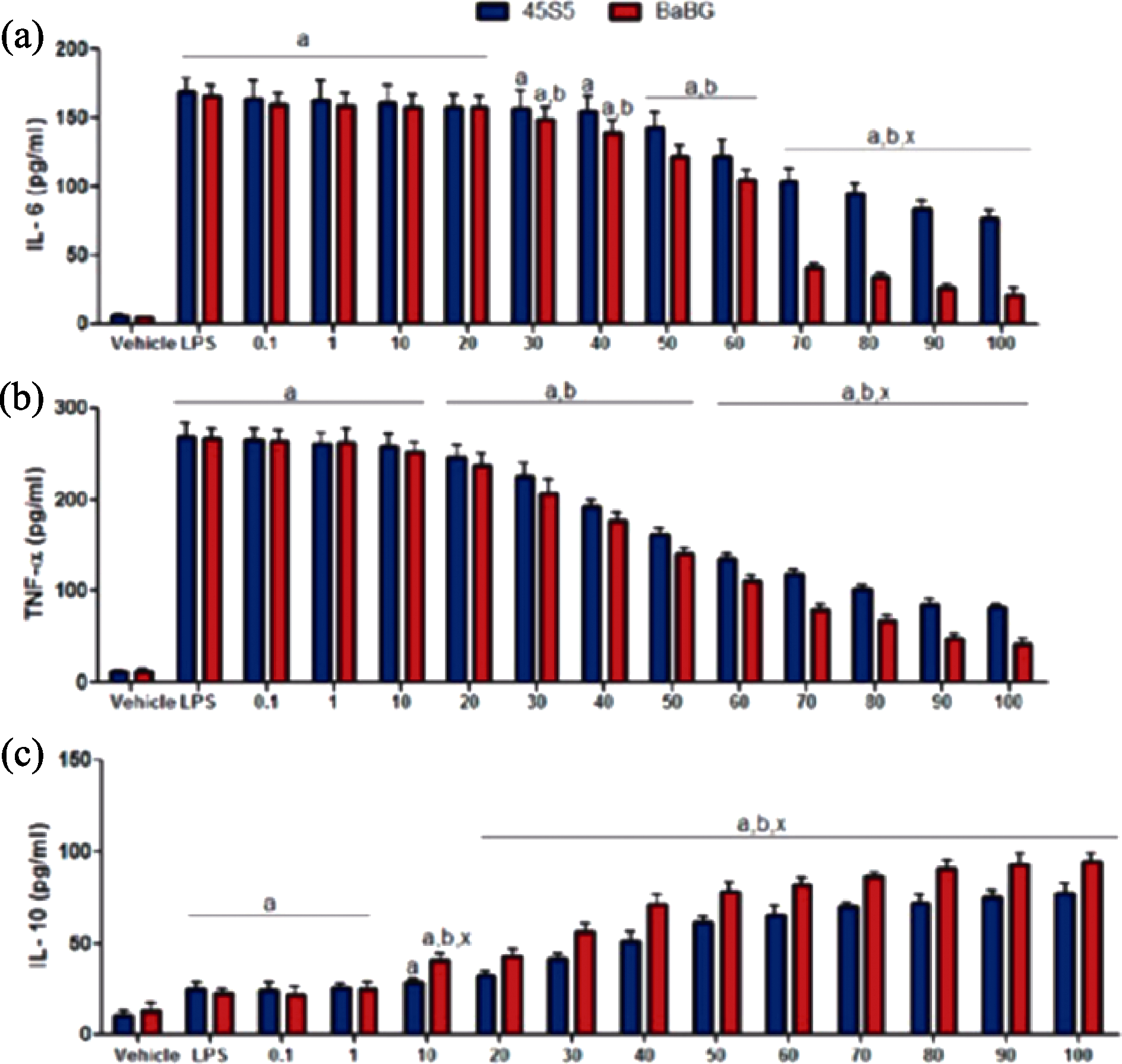
图8 BaBG和45S5对C6细胞因子表达水平的影响[65]
Fig. 8 Effect of BaBG and 45S5 on cytokine expression levels in C6 cells[65] IL-6: Interleukin-6; TNF-α: Tumor necrosis factor-α; IL-10: Interleukin-10
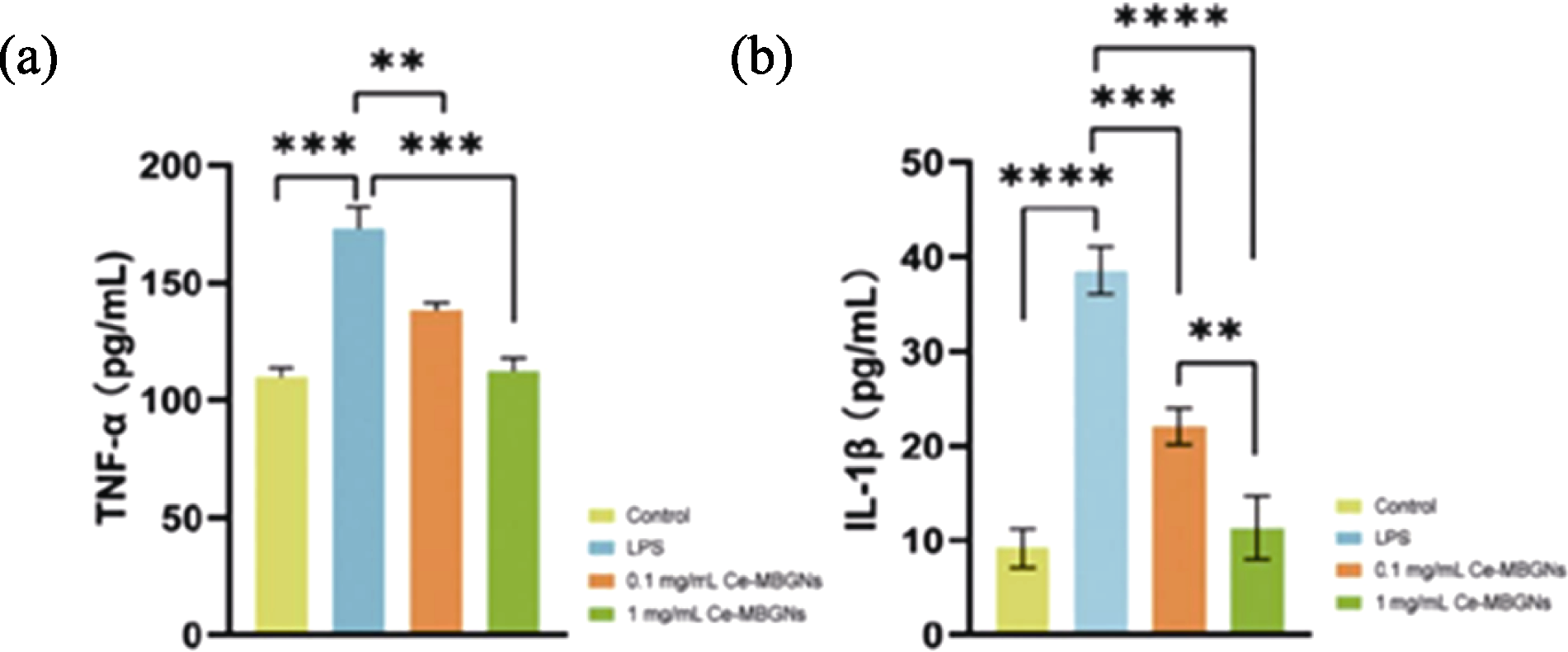
图9 Ce-MBGNs对TNF-α (a)和IL-1β (b)分泌量的影响[67]
Fig. 9 Effect of Ce-MBGNs on the production of TNF-α (a) and IL-1β (b)[67] TNF-α: Tumor necrosis factor-α; IL-1β: Interleukin-1β
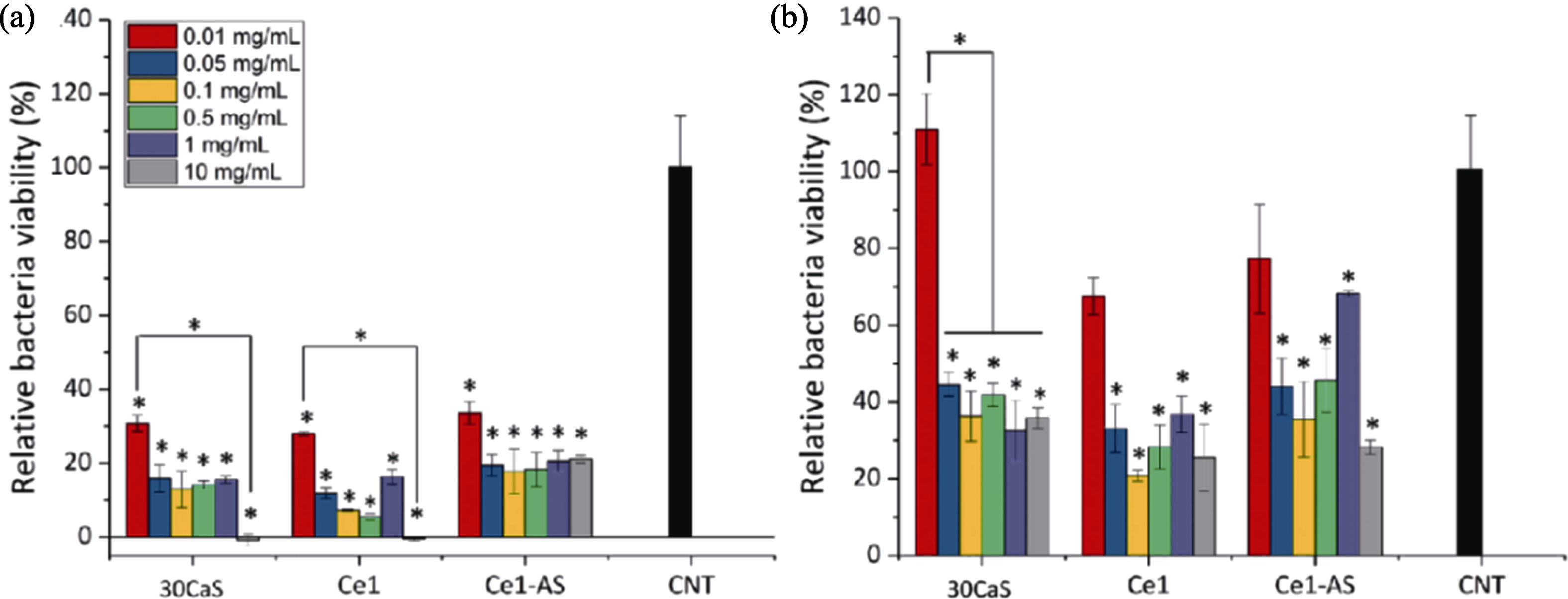
图10 MBGNP对不同细菌的抗菌效果[75]
Fig. 10 Antimicrobial effect of MBGNP on different bacterias[75] (a) S. aureus (Gram-positive); (b) E. coli (Gram-negative) (n=3, *: p<0.05)
| Biological function | Material composition | Mode of action | Ref. |
|---|---|---|---|
| Pro-vascularization | PGA/BGN | Promotion of VEGF expression in fibroblasts | [ |
| BGN | Promotion of VEGF release from fibroblasts | [ | |
| MNBGN | Particle size in the range of 0.5-0.8 mm promoting VEGF expression | [ | |
| Immune cell modulation | BGN | Promoting chemotactic migration of neutrophils | [ |
| Zn-Mn- BGN | Mn and Si ions regulating M2 polarization in macrophages | [ | |
| Zn-BGN | Negative regulation of NF-κB signal | [ | |
| Cu-Zn-BBGN | Immunomodulation of DC viability | [ | |
| Antioxidation | BGN | Si scavenging activity on ROS | [ |
| Ce-MBGNs/CS | Scavenging activity on H2O2 | [ | |
| Anti-inflammatory | Ba-BGN | Elevation of anti-inflammatory cytokine IL-10 | [ |
| Ce-MBGNs | Decreasing expression of inflammatory factors TNF-α and IL-1β | [ | |
| Antimicrobial | BGN | High pH and alkaline ions enhancing antimicrobial activity | [ |
| BGN | 58S and 63S for broad-spectrum antibacterial | [ | |
| Ce-MBGNs | Mesoporous structure promoting antimicrobial activity | [ | |
| Cu-MBGNs | Broad-spectrum antimicrobial effect of Cu | [ |
表2 MNBG促进血管化皮肤修复机制
Table 2 Mechanism of MNBG for vascularized skin repair
| Biological function | Material composition | Mode of action | Ref. |
|---|---|---|---|
| Pro-vascularization | PGA/BGN | Promotion of VEGF expression in fibroblasts | [ |
| BGN | Promotion of VEGF release from fibroblasts | [ | |
| MNBGN | Particle size in the range of 0.5-0.8 mm promoting VEGF expression | [ | |
| Immune cell modulation | BGN | Promoting chemotactic migration of neutrophils | [ |
| Zn-Mn- BGN | Mn and Si ions regulating M2 polarization in macrophages | [ | |
| Zn-BGN | Negative regulation of NF-κB signal | [ | |
| Cu-Zn-BBGN | Immunomodulation of DC viability | [ | |
| Antioxidation | BGN | Si scavenging activity on ROS | [ |
| Ce-MBGNs/CS | Scavenging activity on H2O2 | [ | |
| Anti-inflammatory | Ba-BGN | Elevation of anti-inflammatory cytokine IL-10 | [ |
| Ce-MBGNs | Decreasing expression of inflammatory factors TNF-α and IL-1β | [ | |
| Antimicrobial | BGN | High pH and alkaline ions enhancing antimicrobial activity | [ |
| BGN | 58S and 63S for broad-spectrum antibacterial | [ | |
| Ce-MBGNs | Mesoporous structure promoting antimicrobial activity | [ | |
| Cu-MBGNs | Broad-spectrum antimicrobial effect of Cu | [ |
| [1] | ZHENG K, TORRE E, BARI A, et al. Antioxidant mesoporous Ce-doped bioactive glass nanoparticles with anti-inflammatory and pro-osteogenic activities. Materials Today Bio, 2020, 5: 100041. |
| [2] | SKALLEVOLD H E, ROKAYA D, KHURSHID Z, et al. Bioactive glass applications in dentistry. International Journal of Materials Science, 2019, 20: 5960. |
| [3] |
MAJUMDAR S, GUPTA S, KRISHNAMURTHY S. Multifarious applications of bioactive glasses in soft tissue engineering. Biomaterials Science, 2021, 9: 8111.
DOI PMID |
| [4] | HONG Z, REIS R L, MANO J F. Preparation and in vitro characterization of scaffolds of poly(L-lactic acid) containing bioactive glass ceramic nanoparticles. Acta Biomaterialia, 2008, 4: 1297. |
| [5] |
REZWAN K, CHEN Q Z, BLAKER J J, et al. Biodegradable and bioactive porous polymer/inorganic composite scaffolds for bone tissue engineering. Biomaterials, 2006, 27: 3413.
DOI PMID |
| [6] | HU Q, JIANG W, LI Y, et al. The effects of morphology on physicochemical properties, bioactivity and biocompatibility of micro-/nano-bioactive glasses. Advanced Powder Technology, 2018, 29: 1812. |
| [7] |
HUANG X L, TENG X, CHEN D, et al. The effect of the shape of mesoporous silica nanoparticles on cellular uptake and cell function. Biomaterials, 2010, 31: 438.
DOI PMID |
| [8] | LI H, LI D, WANG X, et al. Progress in biomaterials-enhanced vascularization by modulating physical properties. ACS Biomaterials Science & Engineering, 2025, 11: 33. |
| [9] |
ALOUI C, PRIGENT A, SUT C, et al. The signaling role of CD40 ligand in platelet biology and in platelet component transfusion. International Journal of Molecular Sciences, 2014, 15(12): 22342.
DOI PMID |
| [10] |
CHAKRABARTI S, RIZVI M, MORIN K, et al. The role of CD40L and VEGF in the modulation of angiogenesis and inflammation. Vascular Pharmacology, 2010, 53: 130.
DOI PMID |
| [11] |
PHILLIPSON M, KUBES P. The healing power of neutrophils. Trends in Immunology, 2019, 40: 635.
DOI PMID |
| [12] |
ZHENG K, NIU W, LEI B, et al. Immunomodulatory bioactive glasses for tissue regeneration. Acta Biomaterialia, 2021, 133: 168.
DOI PMID |
| [13] | MUGHAL A, GILLANI S M H, AHMED S, et al. 3D-printed polyether-ether ketone/carboxymethyl cellulose scaffolds coated with Zn-Mn doped mesoporous bioactive glass nanoparticles. Journal of the Mechanical Behavior of Biomedical Materials, 2024, 156: 106581. |
| [14] | POLO-MONTALVO A, CASARRUBIOS L, SERRANO M C, et al. Effective actions of ion release from mesoporous bioactive glass and macrophage mediators on the differentiation of osteoprogenitor and endothelial progenitor cells. Pharmaceutics, 2021, 13(8):1152. |
| [15] | VARMETTE E A, NOWALK J R, FLICK L M, et al. Abrogation of the inflammatory response in LPS-stimulated RAW 264.7 murine macrophages by Zn- and Cu-doped bioactive Sol-Gel glasses. Journal of Biomedical Materials Research Part A, 2009, 90A: 317. |
| [16] |
WANG L, WEI X, WANG Y. Promoting angiogenesis using immune cells for tissue-engineered vascular grafts. Annals of Biomedical Engineering, 2023, 51: 660.
DOI PMID |
| [17] | SOZZANI S, RUSNATI M, RIBOLDI E, et al. Dendritic cell- endothelial cell cross-talk in angiogenesis. Trends in Immunology, 2007, 28: 385. |
| [18] | ZARUBOVA J, HASANI-SADRABADI M M, ARDEHALI R, et al. Immunoengineering strategies to enhance vascularization and tissue regeneration. Advanced Drug Delivery Reviews, 2022, 184: 114233. |
| [19] |
SOLANKI A K, LALI F V, AUTEFAGE H, et al. Bioactive glasses and electrospun composites that release cobalt to stimulate the HIF pathway for wound healing applications. Biomaterials Research, 2021, 25: 1.
DOI PMID |
| [20] |
JIANG Y, LI Y, LI J, et al. A mussel-inspired extracellular matrix-mimicking composite scaffold for diabetic wound healing. ACS Applied Bio Materials, 2020, 3: 4052.
DOI PMID |
| [21] |
LI H, CHANG J. Stimulation of proangiogenesis by calcium silicate bioactive ceramic. Acta Biomaterialia, 2013, 9: 5379.
DOI PMID |
| [22] |
DAY R M, BOCCACCINI A R, SHUREY S, et al. Assessment of polyglycolic acid mesh and bioactive glass for soft-tissue engineering scaffolds. Biomaterials, 2004, 25: 5857.
PMID |
| [23] |
LI R, CLARK A E, HENCH L L. An investigation of bioactive glass powders by Sol-Gel processing. Journal of Applied Biomaterials, 1991, 2: 231.
PMID |
| [24] | LIN C, MAO C, ZHANG J J, et al. Healing effect of bioactive glass ointment on full-thickness skin wounds. Biomedical Materials, 2012, 7: 045017. |
| [25] | LU Y, YANG Y, XIAO L, et al. Autocrine and paracrine effects of vascular endothelial cells promote cutaneous wound healing. BioMed Research International, 2021, 10: 6695663. |
| [26] | JIN L, LONG Y, ZHANG Q, et al. MiRNAs regulate cell communication in osteogenesis-angiogenesis coupling during bone regeneration. Molecular Biology Reports, 2023, 50: 8715. |
| [27] |
HOPPE A, GÜLDAL N S, BOCCACCINI A R. A review of the biological response to ionic dissolution products from bioactive glasses and glass-ceramics. Biomaterials, 2011, 32: 2757.
DOI PMID |
| [28] |
WU C T, ZHOU Y H, XU M C, et al. Copper-containing mesoporous bioactive glass scaffolds with multifunctional properties of angiogenesis capacity, osteostimulation and antibacterial activity. Biomaterials, 2013, 34: 422.
DOI PMID |
| [29] |
WU C T, ZHOU Y H, FAN W, et al. Hypoxia-mimicking mesoporous bioactive glass scaffolds with controllable cobalt ion release for bone tissue engineering. Biomaterials, 2012, 33: 2076.
DOI PMID |
| [30] |
PATEL U, MOSS R M, HOSSAIN K M Z, et al. Structural and physico-chemical analysis of calcium/strontium substituted, near-invert phosphate based glasses for biomedical applications. Acta Biomaterialia, 2017, 60: 109.
DOI PMID |
| [31] | BOCCARDI E, CIRALDO F E, BOCCACCINI A R. Bioactive glass-ceramic scaffolds: processing and properties. MRS Bulletin, 2017, 42: 226. |
| [32] | LEU A, LEACH J K. Proangiogenic potential of a collagen/ bioactive glass substrate. Pharmaceutical Research, 2008, 25: 1222. |
| [33] | LIN Y, XIAO W, LIU X, et al. Long-term bone regeneration, mineralization and angiogenesis in rat calvarial defects implanted with strong porous bioactive glass (13-93) scaffolds. Journal of Non-Crystalline Solids, 2016, 432: 120. |
| [34] | LI Y, CHEN L, CHEN X, et al. High phosphate content in bioactive glasses promotes osteogenesis in vitro and in vivo. Dental Materials, 2021, 37: 272. |
| [35] | GERHARDT L C, WIDDOWS K L, EROL M M, et al. The pro-angiogenic properties of multi-functional bioactive glass composite scaffolds. Biomaterials, 2011, 32: 4096. |
| [36] |
DETSCH R, STOOR P, GRÜNEWALD A, et al. Increase in VEGF secretion from human fibroblast cells by bioactive glass S53P4 to stimulate angiogenesis in bone. Journal of Biomedical Materials Research Part A, 2014, 102: 4055.
DOI PMID |
| [37] | ZHU Y, MA Z, KONG L, et al. Modulation of macrophages by bioactive glass/sodium alginate hydrogel is crucial in skin regeneration enhancement. Biomaterials, 2020, 256: 120216. |
| [38] | SINGER B D, CHANDEL N S. Immunometabolism of pro-repair cells. The Journal of Clinical Investigation, 2019, 129: 2597. |
| [39] | MARTIN P, LEIBOVICH S J. Inflammatory cells during wound repair: the good, the bad and the ugly. Trends Cell Biology, 2005, 15: 599. |
| [40] |
AHMADI A R, CHICCO M, HUANG J, et al. Stem cells in burn wound healing: a systematic review of the literature. Burns, 2019, 45: 1014.
DOI PMID |
| [41] | WANG S, YANG J, ZHAO G, et al. Current applications of platelet gels in wound healing: a review. Wound Repair and Regeneration, 2021, 29: 370. |
| [42] |
SUMMERS C, RANKIN S M, CONDLIFFE A M, et al. Neutrophil kinetics in health and disease. Trends in Immunology, 2010, 31: 318.
DOI PMID |
| [43] |
BURN G L, FOTI A, MARSMAN G, et al. The neutrophil. Immunity, 2021, 54: 1377.
DOI PMID |
| [44] | BASHIR S, SHARMA Y, ELAHI A, et al. Macrophage polarization: the link between inflammation and related diseases. Inflammatory Research, 2016, 65: 1. |
| [45] | YUNNA C, MENGRU H, LEI W, et al. Macrophage M1/M2 polarization. European Journal of Pharmacology, 2020, 877: 173090. |
| [46] |
SPILLER K L, ANFANG R R, SPILLER K J, et al. The role of macrophage phenotype in vascularization of tissue engineering scaffolds. Biomaterials, 2014, 35: 4477.
DOI PMID |
| [47] |
GRANEY P L, BEN-SHAUL S, LANDAU S, et al. Macrophages of diverse phenotypes drive vascularization of engineered tissues. Science Advances, 2020, 6: 6391.
DOI PMID |
| [48] |
KREIMENDAHL F, MARQUARDT Y, APEL C, et al. Macrophages significantly enhance wound healing in a vascularized skin model. Journal of Biomedical Materials Research Part A, 2019, 107: 1340.
DOI PMID |
| [49] | YANG M, MA C, LIU S, et al. HIF-dependent induction of adenosine receptor A2b skews human dendritic cells to a Th2-stimulating phenotype under hypoxia. Immunology & Cell Biology, 2010, 88: 165. |
| [50] | BAI W K, ZHANG W, HU B. Vascular endothelial growth factor suppresses dendritic cells function of human prostate cancer. OncoTargets and Therapy, 2018, 11: 1267. |
| [51] | SCHUHLADEN K, STICH L, SCHMIDT J, et al. Cu, Zn doped borate bioactive glasses: antibacterial efficacy and dose-dependent in vitro modulation of murine dendritic cells. Biomaterials Science, 2020, 8: 2143. |
| [52] |
KWEE B J, BUDINA E, NAJIBI A J, et al. CD4 T-cells regulate angiogenesis and myogenesis. Biomaterials, 2018, 178: 109.
DOI PMID |
| [53] |
RAUSCHENBERGER T, SCHMITT V, AZEEM M, et al. T cells control chemokine secretion by keratinocytes. Frontiers in Immunology, 2019, 10: 1917.
DOI PMID |
| [54] | GROME H N, BARNETT L, HAGAR C C, et al. Association of T cell and macrophage activation with arterial vascular health in HIV. AIDS Research and Human Retroviruses, 2016, 33: 181. |
| [55] | KIM E J, BU S Y, SUNG M K, et al. Analysis of antioxidant and anti-inflammatory activity of silicon in murine macrophages. Biological Trace Element Research, 2013, 156: 329. |
| [56] | LIU W, CHEN M, LUO M, et al. Bioactive glass ions hydrogels with antiinflammation antioxidant capacity for treating inflammation- related diseases. Materials & Design, 2023, 227: 111669. |
| [57] |
NIELSEN F H. A novel silicon complex is as effective as sodium metasilicate in enhancing the collagen-induced inflammatory response of silicon-deprived rats. Journal of Trace Elements in Medicine and Biology, 2008, 22: 39.
DOI PMID |
| [58] |
BIRBEN E, SAHINER U M, SACKESEN C, et al. Oxidative stress and antioxidant defense. World Allergy Organization Journal, 2012, 5: 9.
DOI PMID |
| [59] | XU W, QIN Z, XU R, et al. Injectable, pro-osteogenic and antioxidant composite microspheres composed of cerium- containing mesoporous bioactive glass and chitosan for bone regeneration applications. Ceramics International, 2023, 49: 25757. |
| [60] | ZHU Y, ZHANG X, CHANG G, et al. Bioactive glass in tissue regeneration: unveiling recent advances in regenerative strategies and applications. Advanced Materials, 2025, 37: 2312964. |
| [61] |
LOSI P, BRIGANTI E, ERRICO C, et al. Fibrin-based scaffold incorporating VEGF- and bFGF-loaded nanoparticles stimulates wound healing in diabetic mice. Acta Biomaterialia, 2013, 9: 7814.
DOI PMID |
| [62] | FRANK S, HÜBNER G, BREIER G, et al. Regulation of vascular endothelial growth factor expression in cultured keratinocytes. Journal of Biological Chemistry, 1995, 270: 12607. |
| [63] | EL-FIQI A, ALLAM R, KIM H W. Antioxidant cerium ions- containing mesoporous bioactive glass ultrasmall nanoparticles: structural, physico-chemical, catalase-mimic and biological properties. Colloids and Surfaces B: Biointerfaces, 2021, 206: 111932. |
| [64] | EBERSBERGER A, SCHAIBLE H G. Do cytokines play a role in the transition from acute to chronic musculoskeletal pain. Pharmacological Research, 2025, 212: 107585. |
| [65] | MAJUMDAR S, HIRA S K, TRIPATHI H, et al. Synthesis and characterization of barium-doped bioactive glass with potential anti- inflammatory activity. Ceramics International, 2021, 47: 7143. |
| [66] |
JUNG H, LEE H, KIM D, et al. Differential regional vulnerability of the brain to mild neuroinflammation induced by systemic LPS treatment in mice. Journal of Inflammation Research, 2022, 15: 3053.
DOI PMID |
| [67] | DUAN Y, ZHENG K, HU W, et al. Anti-inflammatory cerium- containing nano-scaled mesoporous bioactive glass for promoting regenerative capability of dental pulp cells. International Endodontic Journal, 2024, 57: 727. |
| [68] |
KANG Y, LIU K, CHEN Z, et al. Healing with precision: a multi-functional hydrogel-bioactive glass dressing boosts infected wound recovery and enhances neurogenesis in the wound bed. Journal of Controlled Release, 2024, 370: 210.
DOI PMID |
| [69] | ZHANG D, LEPPÄRANTA O, MUNUKKA E, et al. Antibacterial effects and dissolution behavior of six bioactive glasses. Journal of Biomedical Materials Research Part A, 2010, 93A: 475. |
| [70] | ZEHNDER M, WALTIMO T, SENER B, et al. Dentin enhances the effectiveness of bioactive glass S53P4 against a strain of Enterococcus faecalis. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontoligy, 2006, 101: 530. |
| [71] | MORTAZAVI V, NAHRKHALAJI M M, FATHI M H, et al. Antibacterial effects of Sol-Gel-derived bioactive glass nanoparticle on aerobic bacteria. Journal of Biomedical Materials Research Part A, 2010, 94A: 160. |
| [72] | HU G, XIAO L, TONG P, et al. Antibacterial hemostatic dressings with nanoporous bioglass containing silver. International Journal Nanomedicine, 2012; 7: 2613. |
| [73] | HAN X, CHEN Y, JIANG Q, et al. Novel bioactive glass-modified hybrid composite resin: mechanical properties, biocompatibility, and antibacterial and remineralizing activity. Frontiers in Bioengineering and Biotechnology, 2021, 9: 661734. |
| [74] | ÖZARSLAN A C. Preparation of biosilica glass-based porous scaffolds using various elements (Mg-Zn, Mg-Cu, and Sr-Cu) as bioactive glass co-dopants: in vitro bioactivity and biocompatibility behaviors. Journal of Materials Research, 2023, 38: 3874. |
| [75] | KURTULDU F, KAŇKOVÁ H, BELTRÁN A M, et al. Anti- inflammatory and antibacterial activities of cerium-containing mesoporous bioactive glass nanoparticles for drug-free biomedical applications. Materials Today Bio, 2021, 12: 100150. |
| [76] | POP O L, MESAROS A, VODNAR D C, et al. Cerium oxide nanoparticles and their efficient antibacterial application in vitro against gram-positive and gram-negative pathogens. Nanomaterials, 2020, 10: 1614. |
| [77] | MUTLU N, KURTULDU F, UNALAN I, et al. Effect of Zn and Ga doping on bioactivity, degradation, and antibacterial properties of borate 1393-B3 bioactive glass. Ceramics International, 2022, 48: 16404. |
| [78] | LI T, WANG Y, LEI B. Photothermal-antibacterial bioactive noncrystalline nanosystem promotes infected wound tissue regeneration through thermo-ions activation. Chemical Engineering Journal, 2024, 491: 151799. |
| [1] | 余升阳, 苏海军, 姜浩, 余明辉, 姚佳彤, 杨培鑫. 激光增材制造超高温氧化物陶瓷孔隙缺陷形成及抑制研究进展[J]. 无机材料学报, 2025, 40(9): 944-956. |
| [2] | 刘江平, 管鑫, 唐振杰, 朱文杰, 罗永明. 含氮挥发性有机化合物催化氧化的研究进展[J]. 无机材料学报, 2025, 40(9): 933-943. |
| [3] | 肖晓琳, 王玉祥, 谷佩洋, 朱圳荣, 孙勇. 二维无机材料调控病损皮肤组织再生的研究进展[J]. 无机材料学报, 2025, 40(8): 860-870. |
| [4] | 马景阁, 吴成铁. 无机生物材料用于毛囊和毛发再生的研究[J]. 无机材料学报, 2025, 40(8): 901-910. |
| [5] | 张洪健, 赵梓壹, 吴成铁. 无机生物材料调控神经细胞功能及神经化组织再生的研究进展[J]. 无机材料学报, 2025, 40(8): 849-859. |
| [6] | 王宇彤, 常江, 徐合, 吴成铁. 硅酸盐生物陶瓷/玻璃促创面修复的研究进展:作用、机制和应用方式[J]. 无机材料学报, 2025, 40(8): 911-920. |
| [7] | 马文平, 韩雅卉, 吴成铁, 吕宏旭. 无机活性材料在类器官研究领域的应用[J]. 无机材料学报, 2025, 40(8): 888-900. |
| [8] | 罗晓民, 乔志龙, 刘颍, 杨晨, 常江. 无机生物活性材料调控心肌再生的研究进展[J]. 无机材料学报, 2025, 40(8): 871-887. |
| [9] | 朱文杰, 唐璐, 陆继长, 刘江平, 罗永明. 钙钛矿型氧化物催化氧化挥发性有机化合物的研究进展[J]. 无机材料学报, 2025, 40(7): 735-746. |
| [10] | 胡智超, 杨鸿宇, 杨鸿程, 孙成礼, 杨俊, 李恩竹. P-V-L键理论在微波介质陶瓷性能调控中的应用[J]. 无机材料学报, 2025, 40(6): 609-626. |
| [11] | 吴琼, 沈炳林, 张茂华, 姚方周, 邢志鹏, 王轲. 铅基织构压电陶瓷研究进展[J]. 无机材料学报, 2025, 40(6): 563-574. |
| [12] | 张碧辉, 刘小强, 陈湘明. Ruddlesden-Popper结构杂化非常规铁电体的研究进展[J]. 无机材料学报, 2025, 40(6): 587-608. |
| [13] | 吴杰, 杨帅, 王明文, 李景雷, 李纯纯, 李飞. 铅基织构压电陶瓷的发展历程、现状与挑战[J]. 无机材料学报, 2025, 40(6): 575-586. |
| [14] | 姜昆, 李乐天, 郑木鹏, 胡永明, 潘勤学, 吴超峰, 王轲. PZT陶瓷的低温烧结研究进展[J]. 无机材料学报, 2025, 40(6): 627-638. |
| [15] | 田睿智, 兰正义, 殷杰, 郝南京, 陈航榕, 马明. 基于微流控技术的纳米无机生物材料制备: 原理及其研究进展[J]. 无机材料学报, 2025, 40(4): 337-347. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||
