无机材料学报 ›› 2023, Vol. 38 ›› Issue (1): 3-31.DOI: 10.15541/jim20220218 CSTR: 32189.14.10.15541/jim20220218
所属专题: 【信息功能】敏感陶瓷(202506)
• 专栏:抗疫生物材料(特邀编辑: 杨勇) • 上一篇 下一篇
李妍妍1,2( ), 彭宇思1,2, 林成龙1,2, 罗晓莹3, 滕峥4(
), 彭宇思1,2, 林成龙1,2, 罗晓莹3, 滕峥4( ), 张曦4, 黄政仁1,2, 杨勇1,2(
), 张曦4, 黄政仁1,2, 杨勇1,2( )
)
收稿日期:2022-04-12
修回日期:2022-05-03
出版日期:2023-01-20
网络出版日期:2022-06-22
通讯作者:
杨 勇, 研究员. E-mail: yangyong@mail.sic.ac.cn;作者简介:李妍妍(1997-), 女, 博士研究生. E-mail: liyanyan20@mails.ucas.ac.cn
基金资助:
LI Yanyan1,2( ), PENG Yusi1,2, LIN Chenglong1,2, LUO Xiaoying3, TENG Zheng4(
), PENG Yusi1,2, LIN Chenglong1,2, LUO Xiaoying3, TENG Zheng4( ), ZHANG Xi4, HUANG Zhengren1,2, YANG Yong1,2(
), ZHANG Xi4, HUANG Zhengren1,2, YANG Yong1,2( )
)
Received:2022-04-12
Revised:2022-05-03
Published:2023-01-20
Online:2022-06-22
Contact:
YANG Yong, professor. E-mail: yangyong@mail.sic.ac.cn;About author:LI Yanyan (1997-), female, PhD candidate. E-mail: liyanyan20@mails.ucas.ac.cn
Supported by:摘要:
新型冠状病毒肺炎(Corona Virus Disease 2019, COVID-19)疫情大流行引起全球对此重大突发公共卫生事件的高度关注。新型冠状病毒(SARS-CoV-2)经过多次突变, 出现传染速度加快、免疫逃逸、隐匿性传播等特性, 令防控形势至今仍异常严峻。对患者的早发现、早隔离仍然是目前最有效的防控措施。因此, 迫切需要快速、高灵敏的检测手段来甄别此病毒, 以便及早识别感染者。本文简要介绍了SARS-CoV-2的一般特征, 并针对核酸、抗体、抗原及病原体作为检测靶标的不同检测手段及最新进展进行分类概述; 对一些光学、电学、磁学以及可视化的新型纳米传感器在SARS-CoV-2检测技术上的应用进行了分析。鉴于纳米技术的应用在提高检测灵敏度、特异性以及准确率上具有优势, 本文详细介绍了新型纳米传感器在SARS-CoV-2检测中的研究进展, 包括表面增强拉曼基生物传感器、电化学生物传感器、磁纳米生物传感器以及比色生物传感器等, 并探讨了纳米材料在新型生物传感器构建中的作用和挑战, 为纳米材料研究人员开发各种类型的冠状病毒传感技术提供思路。
中图分类号:
李妍妍, 彭宇思, 林成龙, 罗晓莹, 滕峥, 张曦, 黄政仁, 杨勇. 用于新型冠状病毒检测的纳米材料及生物传感技术[J]. 无机材料学报, 2023, 38(1): 3-31.
LI Yanyan, PENG Yusi, LIN Chenglong, LUO Xiaoying, TENG Zheng, ZHANG Xi, HUANG Zhengren, YANG Yong. Nanomaterials and Biosensing Technology for the SARS-CoV-2 Detection[J]. Journal of Inorganic Materials, 2023, 38(1): 3-31.
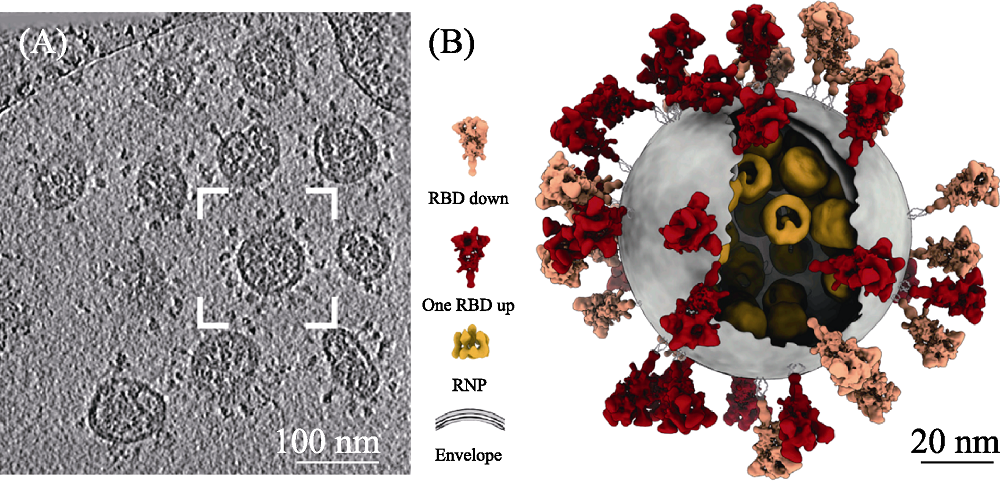
图1 SARS-CoV-2的TEM照片(A)和示意图(B)[9]
Fig. 1 TEM image (A) and schemetic morphology (B) of SARS-CoV-2[9] The color figures can be obtained from online edition
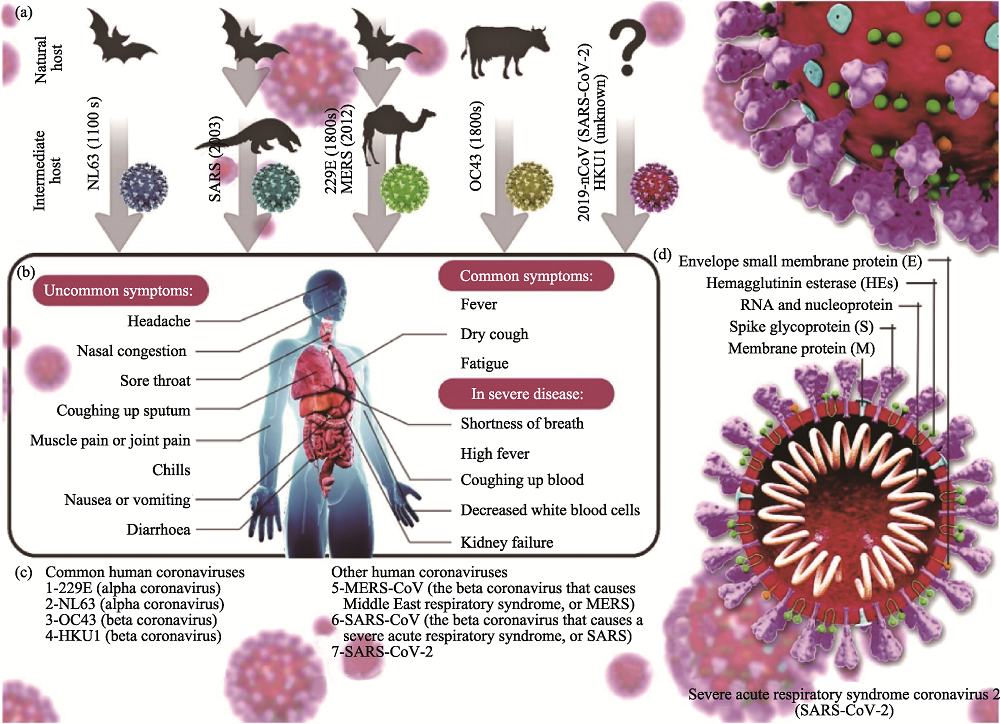
图2 冠状病毒的分类(a、c)、感染症状(b)及其结构示意图(d)[16]
Fig. 2 Classification (a, c), symptoms (b) and structure (c) of coronavirus[16] The color figures can be obtained from online edition
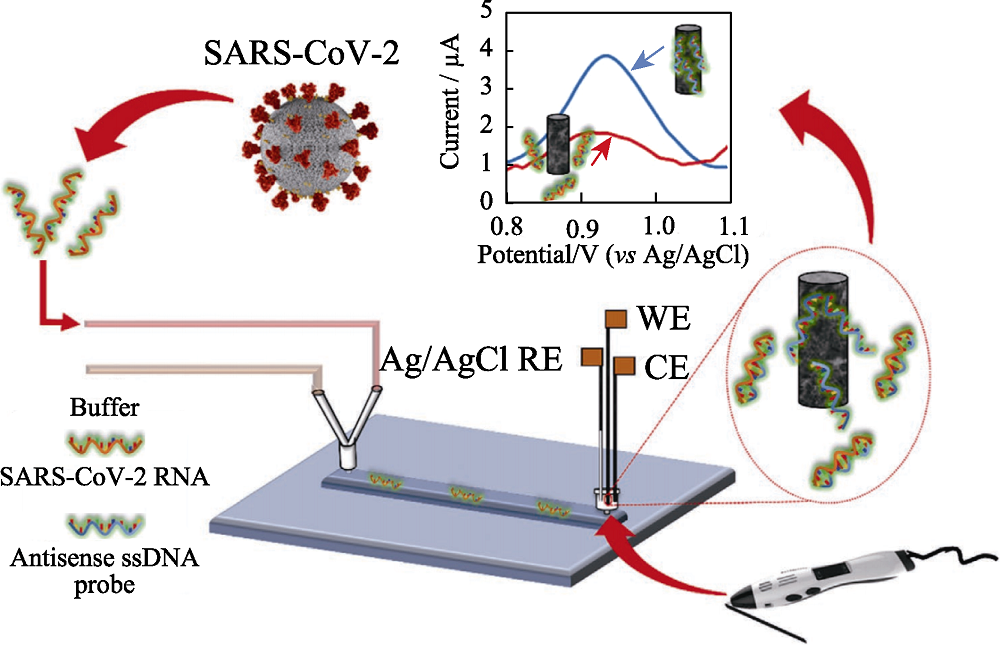
图3 用于检测SARS-CoV-2的微流控基因传感器[35]
Fig. 3 Scheme of the lab-on-a-chip genosensor for SARS- CoV-2 virus detection[35] WE: working electrode; CE: counter electrode; RE: reference electrode; ssDNA: single strand DNA The color figure can be obtained from online edition
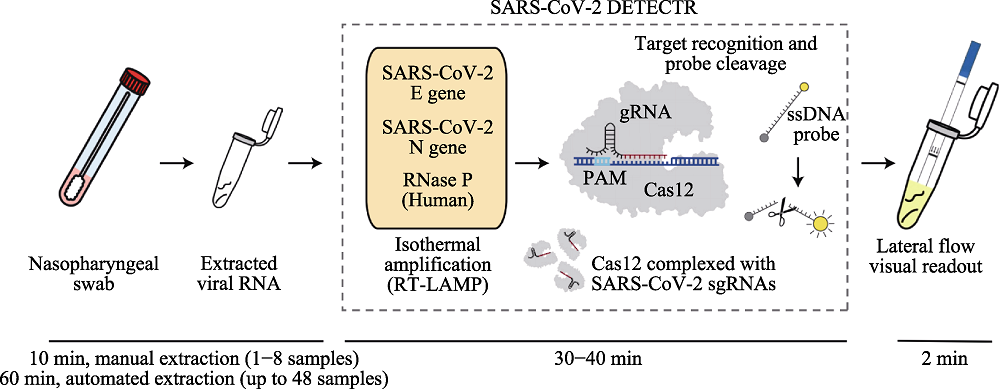
图5 基于CRISPR-Cas12侧向流动技术检测SARS-CoV-2[44]
Fig. 5 Detection of SARS-CoV-2 based on CRISPR-Cas12 combined with lateral flow technique[44] The color figure can be obtained from online edition
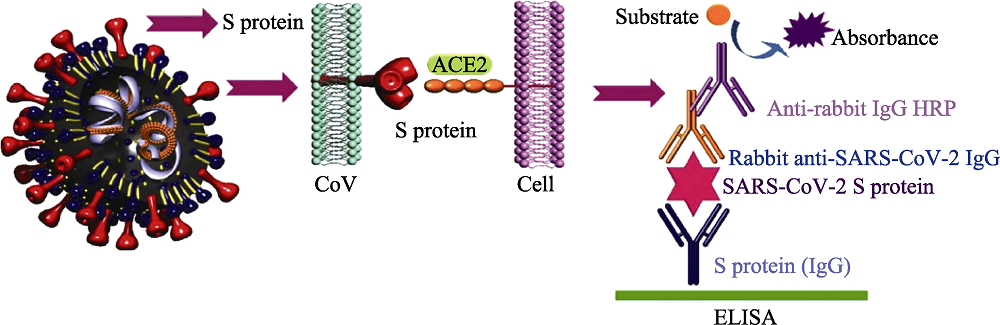
图7 检测SARS-CoV-2的ELISA技术[16]
Fig. 7 ELISA method for detection of SARS-CoV-2[16] ACE2: angiotensin converting enzyme 2; HRP: horse radish peroxidase; ELISA: enzyme linked immunosorbent assay The color figure can be obtained from online edition
| Object sample | Characteristic | Detection technology | Advantage | Disadvantage |
|---|---|---|---|---|
| RNA | 1. Target: the gene sequences of SARS-CoV-2 2. Great producibility 3. Long detection period 4. Possibility of being contaminated and false positive result | Whole genome sequencing | 1. High accuracy and sensitivity 2. Reflecting genetic information of pathogen comprehensively | 1. Expensive special instruments 2. Relying on professionals 3. Difficulty in detection on a large scale |
| RT-qPCR | 1. High sensitivity and specificity 2. Low cost | 1. Long amplification time 2. High requirements of equipment 3. Complex operation | ||
| LAMP | 1. Isothermal reaction 2. High efficiency and speed 3. High sensitivity and visualization | 1. Complex design of primer 2. Low specificity | ||
| Microfluidic chip | 1. Multiple detection of pathogens 2. Integration of sample preparation and detection 3. Ability in automate analysis | Difficulty in chip design, material selection, processing, packaging, and storage | ||
| ddPCR | 1. High sensitivity and lowest limitation of detection 2. Facilitation and high degree of automation 3. Quantitative detection | 1. Small reaction volume 2. Expensive equipment and reagents | ||
| CRISPR | 1. High speed and low cost 2. High sensitivity 3. Strong system stability 4. On-site detection | The accuracy of detection needs to be verified | ||
| Antibodies | 1. Target: human antibodies stimulated by SARS-CoV-2 2. Easy sample collection and low detection threshold 3. Simple operation and high throughput 4. Limitation of timeframe 5. Lower sensitivity and specificity than those of nucleic acid detection | ELISA | 1. Low difficulty of standardization of carrier 2. High sensitivity and specificity 3. Simple equipment | 1. Long detection time and cumbersome steps 2. Limited single detection throughout |
| LFIA (Colloidal gold method) | 1. On-site detection caused by easy operation 2. High sensitivity and speed 3. Low cost 4. Mass production | 1. Only qualitative analysis 2. Different reproducibility of different batches of products | ||
| CLIA | 1. High sensitivity and specificity 2. High throughput detection and high degree of automation | 1. Special instrument 2. High detection cost | ||
| Antigen | 1. Target: SARS-CoV-2 antigen 2. Simple and fast operation | LFIA (Colloidal gold method) | 1. Fast and facile operation 2. Visualization 3. On-site detection and large-scale population screening | Low sensitivity |
表1 常规SARS-CoV-2检测方法比较
Table 1 Comparison of conventional detection methods for SARS-CoV-2
| Object sample | Characteristic | Detection technology | Advantage | Disadvantage |
|---|---|---|---|---|
| RNA | 1. Target: the gene sequences of SARS-CoV-2 2. Great producibility 3. Long detection period 4. Possibility of being contaminated and false positive result | Whole genome sequencing | 1. High accuracy and sensitivity 2. Reflecting genetic information of pathogen comprehensively | 1. Expensive special instruments 2. Relying on professionals 3. Difficulty in detection on a large scale |
| RT-qPCR | 1. High sensitivity and specificity 2. Low cost | 1. Long amplification time 2. High requirements of equipment 3. Complex operation | ||
| LAMP | 1. Isothermal reaction 2. High efficiency and speed 3. High sensitivity and visualization | 1. Complex design of primer 2. Low specificity | ||
| Microfluidic chip | 1. Multiple detection of pathogens 2. Integration of sample preparation and detection 3. Ability in automate analysis | Difficulty in chip design, material selection, processing, packaging, and storage | ||
| ddPCR | 1. High sensitivity and lowest limitation of detection 2. Facilitation and high degree of automation 3. Quantitative detection | 1. Small reaction volume 2. Expensive equipment and reagents | ||
| CRISPR | 1. High speed and low cost 2. High sensitivity 3. Strong system stability 4. On-site detection | The accuracy of detection needs to be verified | ||
| Antibodies | 1. Target: human antibodies stimulated by SARS-CoV-2 2. Easy sample collection and low detection threshold 3. Simple operation and high throughput 4. Limitation of timeframe 5. Lower sensitivity and specificity than those of nucleic acid detection | ELISA | 1. Low difficulty of standardization of carrier 2. High sensitivity and specificity 3. Simple equipment | 1. Long detection time and cumbersome steps 2. Limited single detection throughout |
| LFIA (Colloidal gold method) | 1. On-site detection caused by easy operation 2. High sensitivity and speed 3. Low cost 4. Mass production | 1. Only qualitative analysis 2. Different reproducibility of different batches of products | ||
| CLIA | 1. High sensitivity and specificity 2. High throughput detection and high degree of automation | 1. Special instrument 2. High detection cost | ||
| Antigen | 1. Target: SARS-CoV-2 antigen 2. Simple and fast operation | LFIA (Colloidal gold method) | 1. Fast and facile operation 2. Visualization 3. On-site detection and large-scale population screening | Low sensitivity |
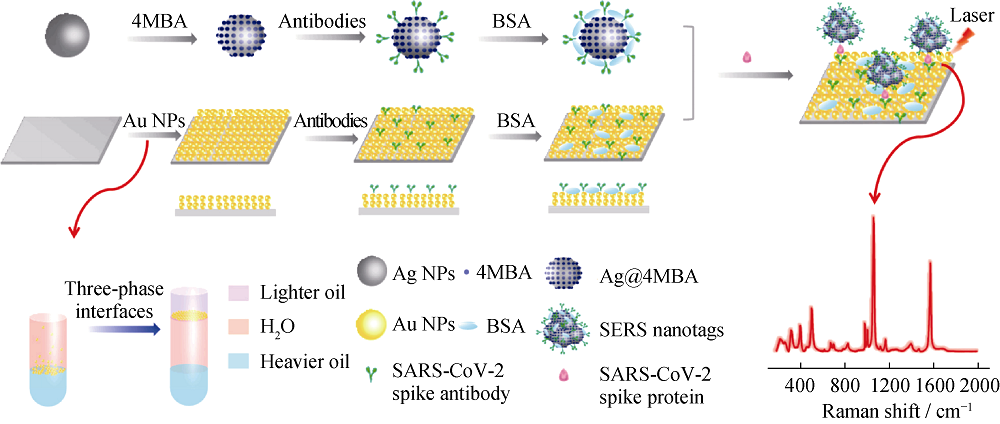
图8 SERS基免疫平台示意图[77]
Fig. 8 Schematic illustration of the SERS-based immunoassay[77] MBA: thiosalicylic acid; BSA: bovine serum albumin; NPs: nanoparticles The color figure can be obtained from online edition
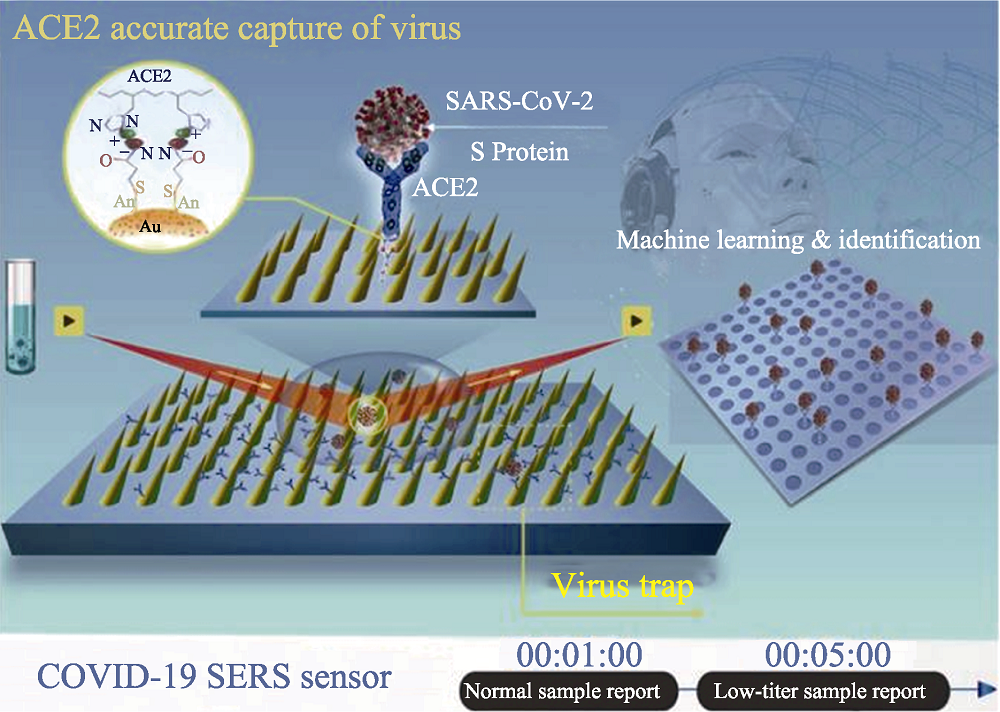
图9 SERS生物传感器精准捕获待检SARS-CoV-2病毒示意图[8]
Fig. 9 Schematic diagram of operation procedure of COVID-19 SERS sensor[8] The color figure can be obtained from online edition
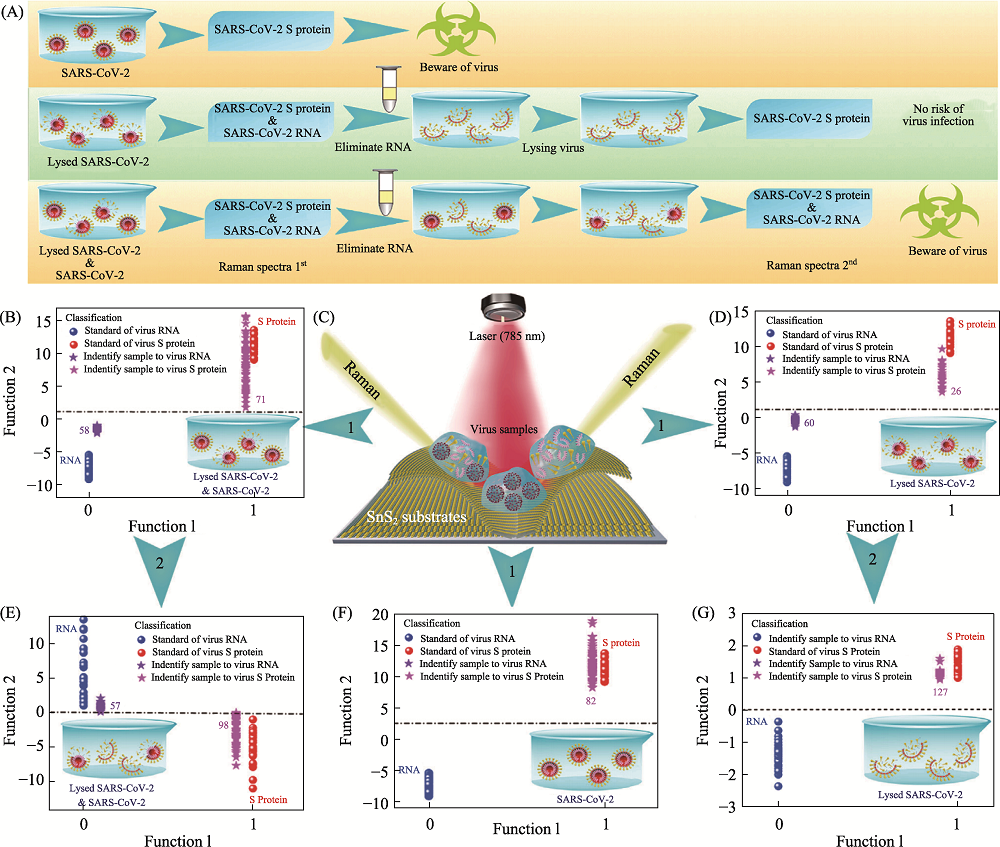
图10 基于SnS2微球的两步SERS检测法诊断SARS-CoV-2活性及其传染性[80]
Fig. 10 Application of SnS2 microspheres for diagnosing the infectiousness of SARS-CoV-2[80] (A) Experimental procedure for diagnosing the infectiousness of SARS-CoV-2; (B) SVM analysis results to identify the mixture of the SARS-CoV-2 with complete viral structure and the lysed SARS-CoV-2; (C) Raman scattering diagram of three contamination situations of the novel coronavirus based on SnS2 substrates; (D) SVM analysis results to identify the lysed SARS-CoV-2; (E) SVM analysis results to identify the mixture of the SARS-CoV-2 with complete viral structure and the lysed SARS-CoV-2 after eliminating RNA and relysing virus samples; (F) SVM analysis results to identify the SARS-CoV-2 with complete viral structure; (G) SVM analysis results to identify the lysed SARS-CoV-2 after eliminating RNA and relysing virus samples. SVM: support vector machine The color figure can be obtained from online edition
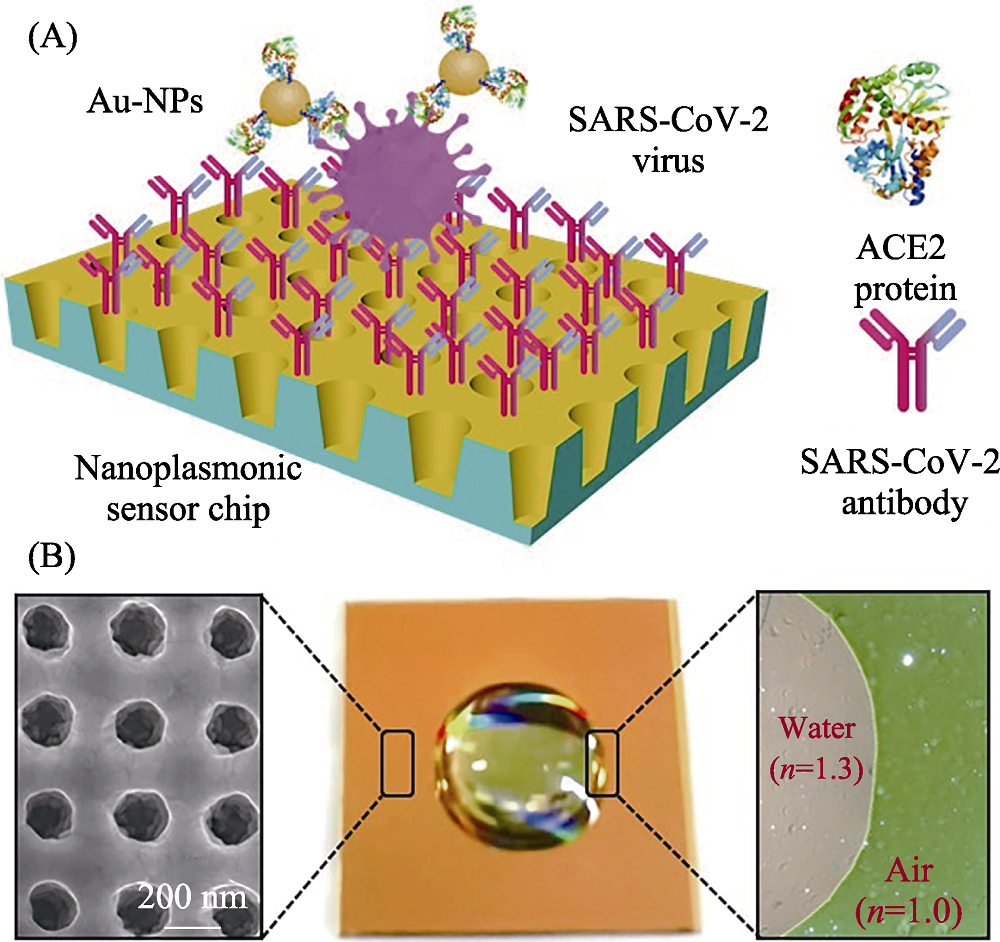
图11 纳米等离子光学传感芯片检测SARS-CoV-2颗粒示意图[89]
Fig. 11 Schematic diagram of nano-plasma optic sensor for detection of SARS-CoV-2[89] (A) Schematic diagram of the nanoplasmonic resonance sensor for determination of SARS-CoV-2 pseudovirus concentration; (B) Photograph (middle) of one piece of Au nanocup array chip with a drop of water on top The color figure can be obtained from online edition
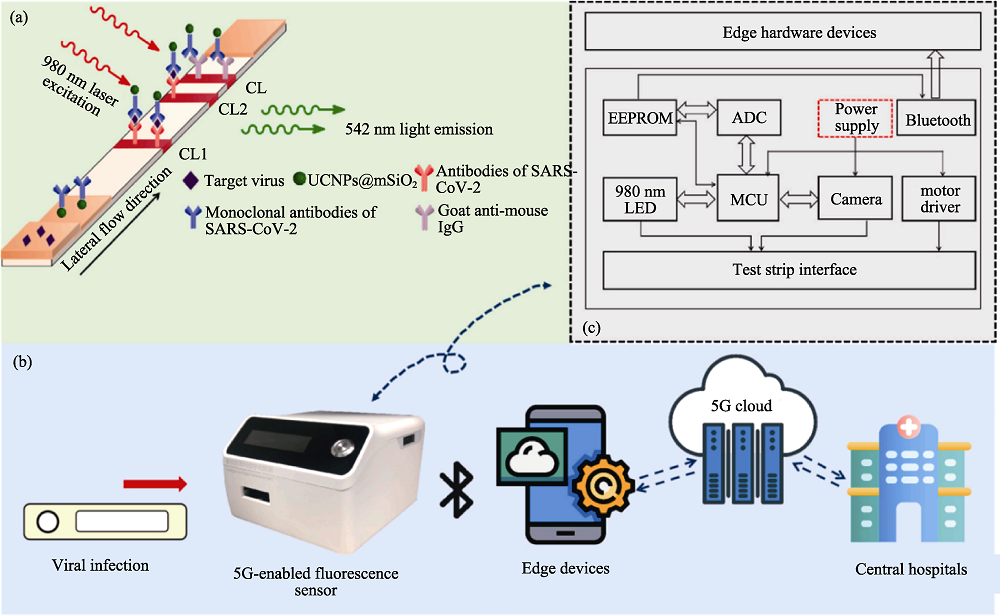
图12 基于5G支持的荧光生物传感器用于SARS-CoV-2检测[100]
Fig. 12 SARS-CoV-2 detection based on 5G-enabled fluorescence biosensor[100] (a) The principle of the UCNPs based lateral flow assay in detection of SARS-CoV-2; (b) The working process of the proposed 5G-enabled fluorescence sensor; (c) The circuit configuration and hardware composition of the fluorescence sensor; CL: control line; TL1: test line 1; TL2: test line 2; UCNPs: up-conversion nanoparticles; EEPROM: electrically erasable programmable read only memory; ADC: application data center; MCU: motor control unit The color figure can be obtained from online edition
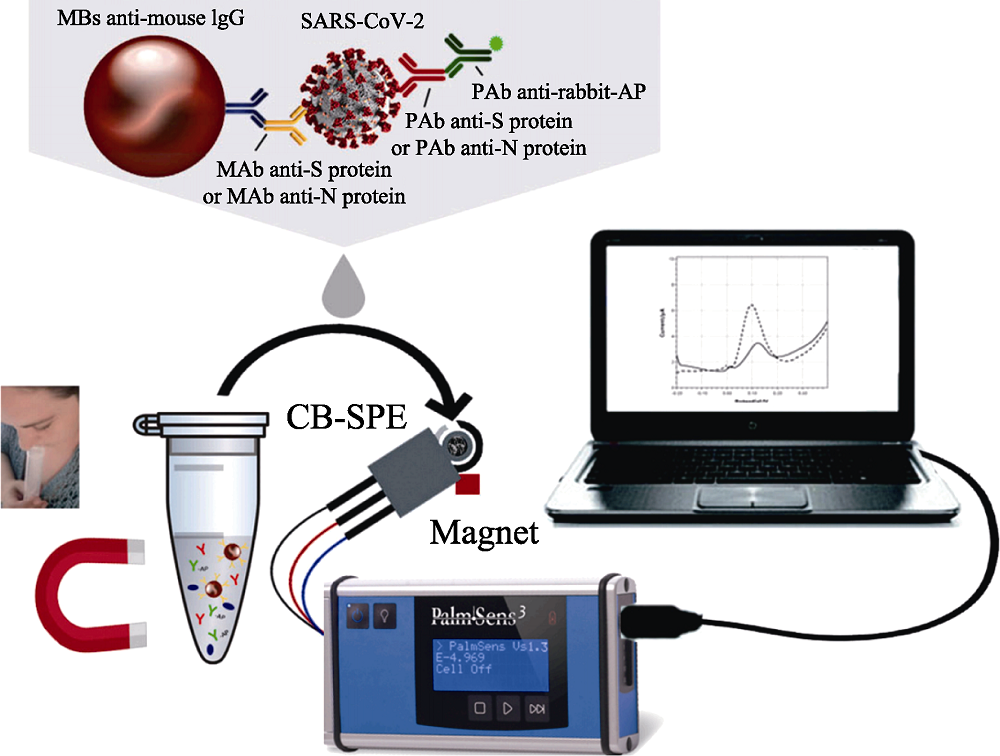
图13 用于检测未处理唾液中SARS-CoV-2的磁珠基电化学分析平台[126]
Fig. 13 Magnetic beads-based electrochemical assay for SARS-CoV-2 detection in untreated saliva[126] MBs: magnetic beads; MAb: monoclonal antibody; PAb: polyclonal antibody; AP: alkaline phosphatase; CB-SPE: carbon-based screen-printed electrodes The color figure can be obtained from online edition
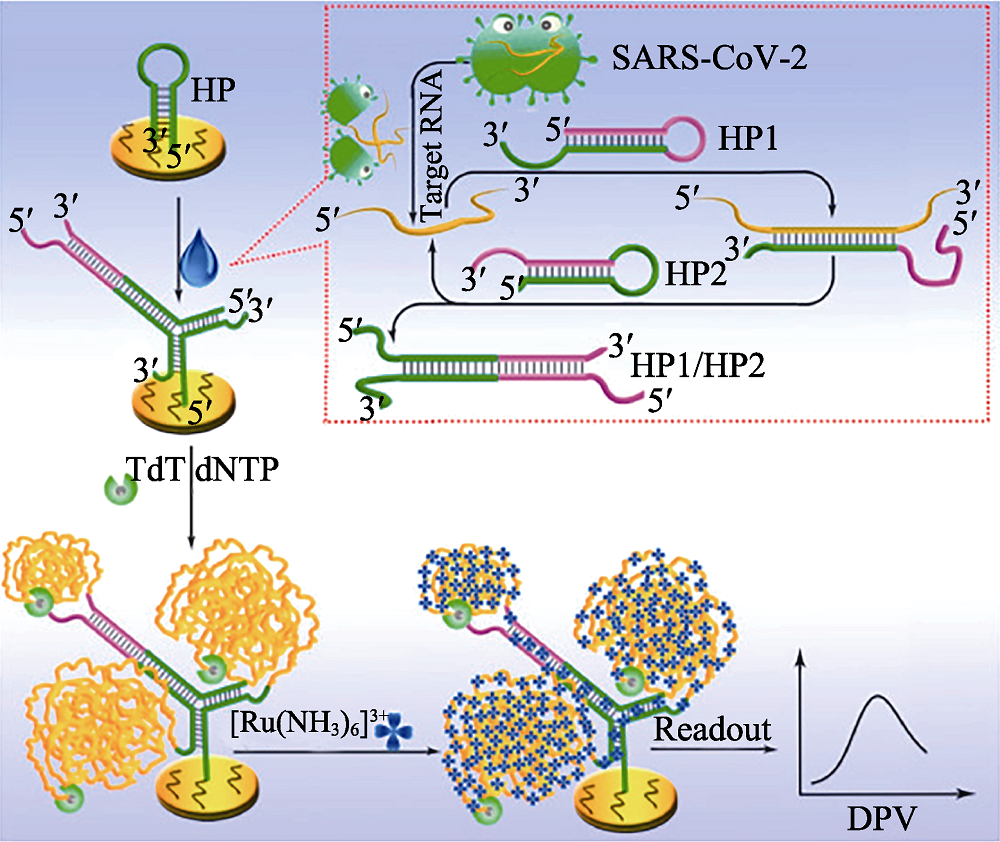
图14 基于电化学生物传感器分析SARS-CoV-2 RNA的检测原理[136]
Fig. 14 Principle of the proposed electrochemical biosensor for sensitive analysis of SARS-CoV-2 RNA[136] HP: hairpin; TdT: terminal deoxynucleotidyl transferase; dNTP: deoxyribonucleotides; DPV: differential pulse voltammetry The color figure can be obtained from online edition
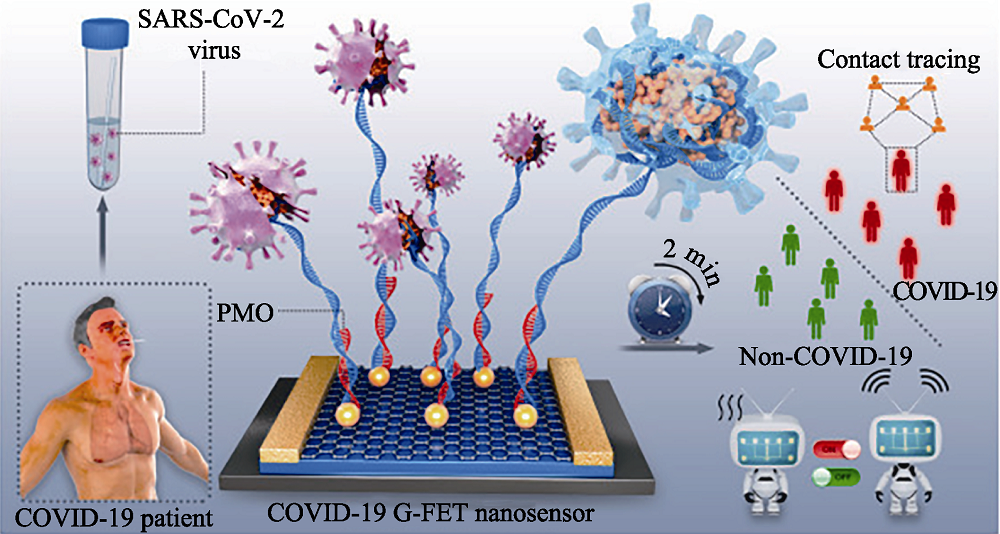
图15 基于PMO修饰的G-FET纳米传感器快速直接识别SARS-CoV-2的示意图[148]
Fig. 15 Schematic diagram of rapid direct identification of SARS-CoV-2 using PMO-functionalized G-FET nano-sensors[148] G-FET: graphene field-effect transistor; PMO: phosphorodiamidate morpholino oligos The color figure can be obtained from online edition
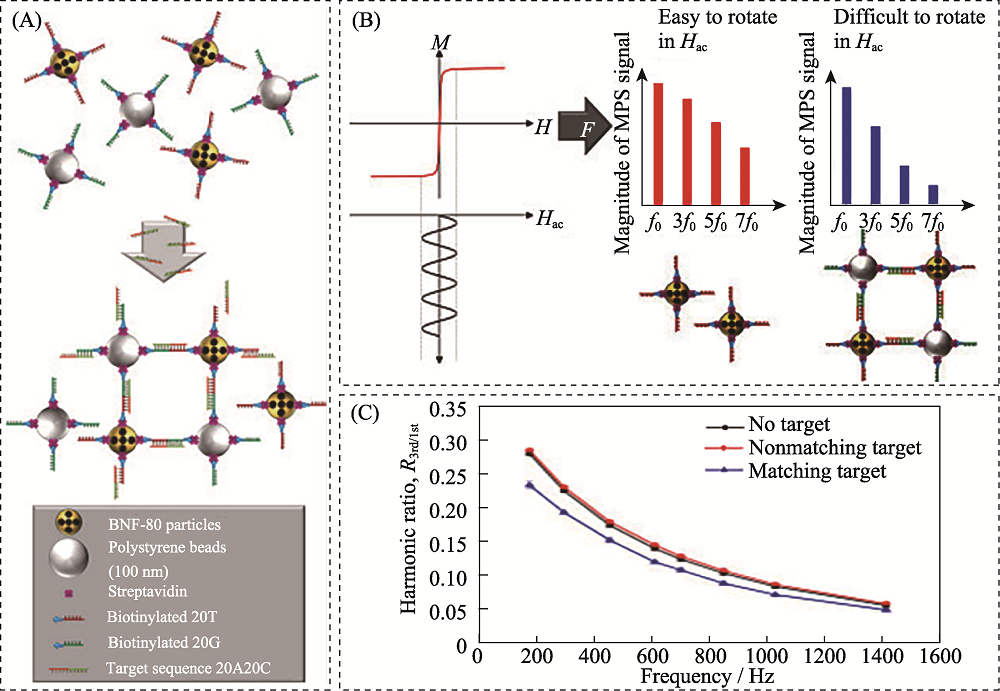
图16 基于磁颗粒光谱生物传感器的SARS-CoV-2核酸检测示意图[166]
Fig. 16 Schematic diagram of detection of SARS-CoV-2 RNA based on magnetic particle spectroscopy biosensors[166] (A) Magnetic nanoparticles (gold) and polystyrene beads (silver) with streptavidin (purple)-modified surface are equipped with single stranded DNA strands (red and green, respectively) with a specific sequence via biotin-streptavidin-binding; (B) Applying a sinusoidal magnetic field (black) to a solution of nanoparticles results in reorientation of the nanoparticles which can be readout by measuring the magnetic response M of the nanoparticles; (C) Exemplary spectrum of the ratio of received harmonics as a function of excitation frequencies for 80 nm BNF magnetic particles The color figure can be obtained from online edition
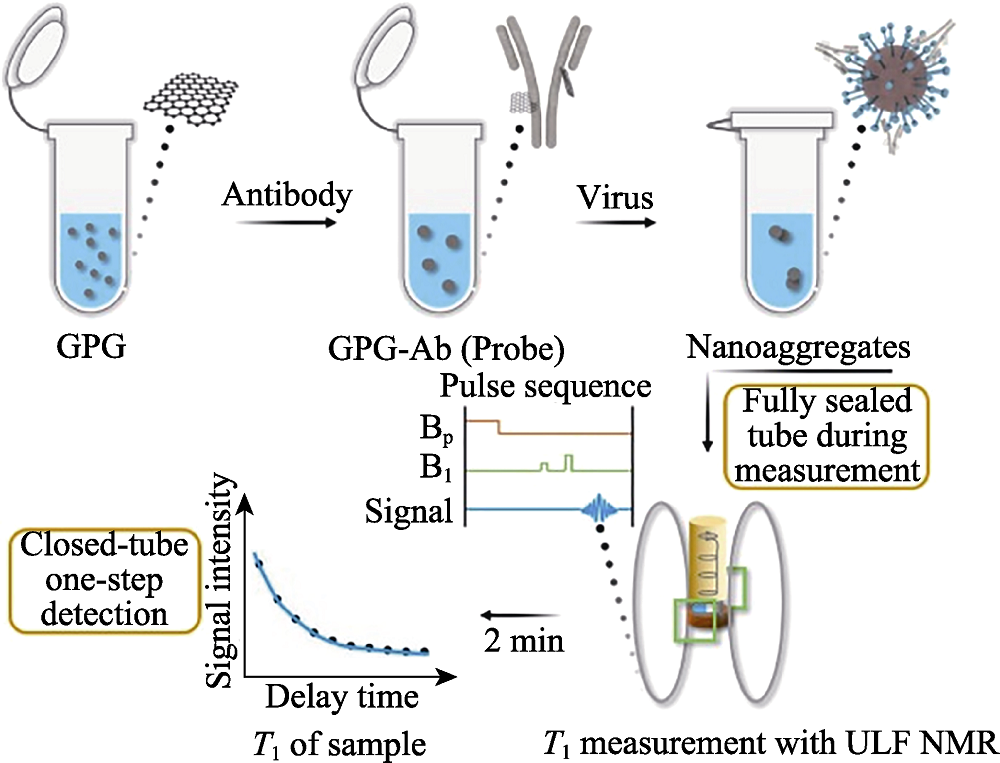
图17 基于超低场核磁共振的磁弛豫开关分析的SARS-CoV-2检测过程[169]
Fig. 17 Detection process of SARS-CoV-2 of the magnetic relaxation switches assay with ULF NMR[169] ULF: ultra-low field; GPG: Gd3+ loaded PEG modified GQDs; GQDs: graphene quantum dots The color figure can be obtained from online edition
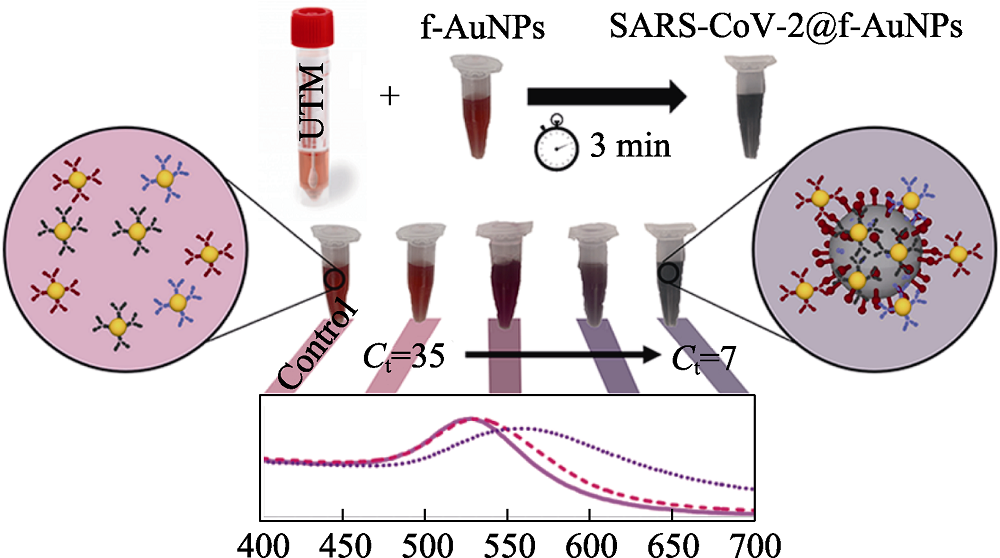
图18 基于比色法的SARS-CoV-2检测示意图[187]
Fig. 18 Schematic diagram of the detection of SARS-CoV-2 based on colorimetric biosensors[187] UTM: universal transport medium The color figure can be obtained from online edition
| Detection technology | Detection method | Object | Sample | Related material | Detection time | Lower detection limit | Ref. |
|---|---|---|---|---|---|---|---|
| SERS-based biosensors | Labelled-SERS | S protein | Lysis solution | Macro/nanostructure Au substrate | 15 min | 10 PFU/mL | [ |
| Label-free SERS | Virus particles | Nasal/throat solution | Macro/nanostructure Au substrate, Au nanoparticles | 15 min | 60 copies/mL | [ | |
| SPR-based biosensors | Combining SPR and LSPR | Pseudovirus particles | N/A | Macro/nanostructure Au substrate, Au nanoparticles | 15 min | 370 vp/mL | [ |
| Fluorescence biosensors | “signal on” mode | RNA | Lysis solution | N/A | 15 samples/ 45 min | 600 copies/mL | [ |
| Electrochemical biosensors | Voltammetric/ amperometric biosensors | RNA | Nasal/throat solution | Au nanoparticles | 5 min | 6900 copies/mL | [ |
| Impedimetric biosensors | Antibodies | Serum | Au nanoparticles | 30 min | N/A | [ | |
| Potentiometric biosensors | Cholinesterase | Blood | Graphene and copper | ~7 s (only detection time) | 7.9 × 10-8 mol/L | [ | |
| FET-based biosensors | RNA | Nasal/throat solution | Graphene | 1 min (only detection time) | 10-20 copies/mL | [ | |
| Magnetic biosensors | Magnetoresistance | Antibodies | Blood | Magnetic nanoparticles | 10 min | 5-10 ng/mL | [ |
| Magnetic particle spectroscopy platforms | S protein and N protein | PBS | Magnetic nanoparticles | N/A | 1.56 nmol/L | [ | |
| Nuclear magnetic resonance | Antibodies | Blood | Magnetic graphene quantum dot | 2 min | 248 vp/mL | [ | |
| Colorimetric biosensors | Agglomeration of nanoparticles | RNA | N/A | Au nanoparticles | >45 min | 160 fmol/L | [ |
表2 用于SARS-CoV-2检测的新型生物传感器比较
Table 2 Comparison of novel biosensors for SARS-CoV-2 detection
| Detection technology | Detection method | Object | Sample | Related material | Detection time | Lower detection limit | Ref. |
|---|---|---|---|---|---|---|---|
| SERS-based biosensors | Labelled-SERS | S protein | Lysis solution | Macro/nanostructure Au substrate | 15 min | 10 PFU/mL | [ |
| Label-free SERS | Virus particles | Nasal/throat solution | Macro/nanostructure Au substrate, Au nanoparticles | 15 min | 60 copies/mL | [ | |
| SPR-based biosensors | Combining SPR and LSPR | Pseudovirus particles | N/A | Macro/nanostructure Au substrate, Au nanoparticles | 15 min | 370 vp/mL | [ |
| Fluorescence biosensors | “signal on” mode | RNA | Lysis solution | N/A | 15 samples/ 45 min | 600 copies/mL | [ |
| Electrochemical biosensors | Voltammetric/ amperometric biosensors | RNA | Nasal/throat solution | Au nanoparticles | 5 min | 6900 copies/mL | [ |
| Impedimetric biosensors | Antibodies | Serum | Au nanoparticles | 30 min | N/A | [ | |
| Potentiometric biosensors | Cholinesterase | Blood | Graphene and copper | ~7 s (only detection time) | 7.9 × 10-8 mol/L | [ | |
| FET-based biosensors | RNA | Nasal/throat solution | Graphene | 1 min (only detection time) | 10-20 copies/mL | [ | |
| Magnetic biosensors | Magnetoresistance | Antibodies | Blood | Magnetic nanoparticles | 10 min | 5-10 ng/mL | [ |
| Magnetic particle spectroscopy platforms | S protein and N protein | PBS | Magnetic nanoparticles | N/A | 1.56 nmol/L | [ | |
| Nuclear magnetic resonance | Antibodies | Blood | Magnetic graphene quantum dot | 2 min | 248 vp/mL | [ | |
| Colorimetric biosensors | Agglomeration of nanoparticles | RNA | N/A | Au nanoparticles | >45 min | 160 fmol/L | [ |
| [1] |
YUCE M, FILIZTEKIN E, OZKAYA K G. COVID-19 diagnosis-a review of current methods. Biosensors and Bioelectronics, 2021, 172: 112752.
DOI URL |
| [2] |
JI T X, LIU Z W, WANG G Q, et al. Detection of COVID-19: a review of the current literature and future perspectives. Biosensors and Bioelectronics, 2020, 166: 112455.
DOI URL |
| [3] |
XUE X, BALL J K, ALEXANDER C, et al. All surfaces are not equal in contact transmission of SARS-CoV-2. Matter, 2020, 3(5): 1433.
DOI PMID |
| [4] |
CHEN W, CAI B, GENG Z, et al. Reducing false negatives in COVID-19 testing by using microneedle-based oropharyngeal swabs. Matter, 2020, 3(5): 1589.
DOI PMID |
| [5] |
CUI F Y, ZHOU H S. Diagnostic methods and potential portable biosensors for coronavirus disease 2019. Biosensors and Bioelectronics, 2020, 165: 112349.
DOI URL |
| [6] | LIN D C, LIU L, ZHANG M X, et al. Evaluations of the serological test in the diagnosis of 2019 novel coronavirus (SARS-CoV-2) infections during the COVID-19 outbreak. European Journal of Clinical Microbiology & Infectious Diseases, 2020, 39(12): 2271. |
| [7] |
SEO G, LEE G, KIM M J, et al. Correction to rapid detection of COVID-19 causative virus (SARS-CoV-2) in human nasopharyngeal swab specimens using field-effect transistor-based biosensor. ACS Nano, 2020, 14(9): 12257.
DOI PMID |
| [8] |
YANG Y, PENG Y S, LIN C L, et al. Human ACE2-functionalized gold “virus-trap” nanostructures for accurate capture of SARS-CoV-2 and single-virus SERS detection. Nano-Micro Letters, 2021, 13: 109.
DOI URL |
| [9] |
YAO H P, SONG Y T, CHEN Y, et al. Molecular architecture of the SARS-CoV-2 virus. Cell, 2020, 183(3): 730.
DOI PMID |
| [10] |
ZHOU P, YANG X L, WANG X G, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature, 2020, 579(7798): 270.
DOI URL |
| [11] |
LI W H, MOORE J M, VASILIEVA N, et al. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature, 2003, 426: 450.
DOI URL |
| [12] |
HOFMANN H, PYRC K, HOEK V D L, et al. Human coronavirus NL63 employs the severe acute respiratory syndrome coronavirus receptor for cellular entry. Proceedings of the National Academy of Sciences of the United States of America, 2005, 102(22): 7988.
DOI PMID |
| [13] |
LU G W, HU Y W, WANG Q H, et al. Molecular basis of binding between novel human coronavirus MERS-CoV and its receptor CD26. Nature, 2013, 500(7461): 227.
DOI URL |
| [14] |
RAJ V S, MOU H, SMITS S L, et al. Dipeptidyl peptidase 4 is a functional receptor for the emerging human coronavirus-EMC. Nature, 2013, 495 (7440): 251.
DOI URL |
| [15] |
MENACHERY V D, YOUNT B L JR, DEBBINK K, et al. A SARS-like cluster of circulating bat coronaviruses shows potential for human emergence. Nature Medicine, 2015, 21(12): 1508.
DOI PMID |
| [16] |
OROOJI Y, SOHRABI H, HEMMAT N, et al. An overview on SARS-CoV-2 (COVID-19) and other human coronaviruses and their detection capability via amplification assay, chemical sensing, biosensing, immunosensing, and clinical assays. Nano-Micro Letters, 2021, 13: 18.
DOI URL |
| [17] |
TO K K W, TSANG O T Y, LEUNG W S, et al. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. The Lancet Infectious Diseases, 2020, 20(5): 565.
DOI URL |
| [18] |
DONG X, CAO Y Y, LU X X, et al. Eleven faces of coronavirus disease 2019. Allergy, 2020, 75(7): 1699.
DOI PMID |
| [19] | CORMAN V M, LANDT O, KAISER M, et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro surveillnace, 2020, 25(3): 23. |
| [20] |
LU R J, ZHAO X, LI J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. The Lancet, 2020, 395(10224): 565.
DOI URL |
| [21] |
REN L L, WANG Y M, WU Z Q, et al. Identification of a novel coronavirus causing severe pneumonia in human: a descriptive study. Chinese Medical Journal, 2020, 133(9): 1015.
DOI URL |
| [22] |
PEIRIS S M J, PHIL D, YUEN Y K, et al. The severe acute respiratory syndrome. The New England Journal of Medicine, 2003, 349: 2431.
DOI PMID |
| [23] | CHEN L J, LIU W Y, ZHANG Q, et al. RNA based mNGS approach identifies a novel human coronavirus from two individual pneumonia cases in 2019 Wuhan outbreak. Emerging Microbes & Infections, 2020, 9(1): 313. |
| [24] |
SHI M, ZHANG Y Z, HOLMES E C. Meta-transcriptomics and the evolutionary biology of RNA viruses. Virus Research, 2018, 243: 83.
DOI PMID |
| [25] |
SAKAMOTO Y, SEREEWATTANAWOOT S, SUZUKI A. A new era of long-read sequencing for cancer genomics. Journal of Human Genetics, 2020, 65(1): 3.
DOI PMID |
| [26] |
WANG M, FU A S, HU B, et al. Nanopore targeted sequencing for the accurate and comprehensive detection of SARS-CoV-2 and other respiratory viruses. Small, 2020, 16: 2002169.
DOI URL |
| [27] |
NOTOMI T, OKAYAMA H, MASUBUCHI H, et al. Loop-mediated isothermal amplification of DNA. Nucleic Acids Research, 2000, 28: 63.
PMID |
| [28] |
ZHU X, WANG X X, HAN L M, et al. Multiplex reverse transcription loop-mediated isothermal amplification combined with nanoparticle-based lateral flow biosensor for the diagnosis of COVID-19. Biosensors and Bioelectronics, 2020, 166: 112437.
DOI URL |
| [29] |
ZHUANG J J, YIN J X, LV S W, et al. Advanced "lab-on-a-chip" to detect viruses-current challenges and future perspectives. Biosensors and Bioelectronics, 2020, 163: 112291.
DOI URL |
| [30] |
WANG L J, PUMERA M. Recent advances of 3D printing in analytical chemistry: focus on microfluidic, separation, and extraction devices. TRAC Trends in Analytical Chemistry, 2021, 135: 116151.
DOI URL |
| [31] |
WANG G H, TAN J, TANG M H, et al. Binary centrifugal microfluidics enabling novel, digital addressable functions for valving and routing. Lab on a Chip, 2018, 18(8): 1141.
DOI URL |
| [32] |
CHEN J J, KANG Z W, WANG G H, et al. Optofluidic guiding, valving, switching and mixing based on plasmonic heating in a random gold nanoisland substrate. Lab on a Chip, 2015, 15(11): 2504.
DOI PMID |
| [33] |
TANG M H, LOO J F, WANG Y Y, et al. Motor-assisted chip-in-a-tube (MACT): a new 2- and 3-dimensional centrifugal microfluidic platform for biomedical applications. Lab on a Chip, 2017, 17(3): 474.
DOI PMID |
| [34] | TANG M H, WANG G H, KONG S K, et al. A review of biomedical centrifugal microfluidic platforms. Micromachines (Basel), 2016, 7: 26. |
| [35] |
CREVILLEN A G, MAYORGA-MARTINEZ C C, VAGHASIYA J V, et al. 3D-Printed SARS-CoV-2 RNA genosensing microfluidic system. Advanced Materials Technologies, 2022, 7(6): 2101121.
DOI URL |
| [36] |
WIENCKE J K, BRACCI P M, HSUANG G, et al. A comparison of DNA methylation specific droplet digital PCR (ddPCR) and real time qPCR with flow cytometry in characterizing human T cells in peripheral blood. Epigenetics, 2014, 9(10): 1360.
DOI PMID |
| [37] |
CHEN B, JIANG Y F, CAO X H, et al. Droplet digital PCR as an emerging tool in detecting pathogens nucleic acids in infectious diseases. Clinica Chimica Acta, 2021, 517: 156.
DOI PMID |
| [38] |
SEDLAK R H, JEROME K R. Viral diagnostics in the era of digital polymerase chain reaction. Diagnostic Microbiology and Infectious Disease, 2013, 75(1): 1.
DOI PMID |
| [39] |
DONG L H, ZHOU J B, NIU C Y, et al. Highly accurate and sensitive diagnostic detection of SARS-CoV-2 by digital PCR. Talanta, 2021, 224: 121726.
DOI URL |
| [40] | SUO T, LIU X J, GUO M, et al. ddPCR: a more accurate tool for SARS-CoV-2 detection in low viral load specimens. Emerging Microbes & Infections, 2020, 9: 1259. |
| [41] | HOU T Y, ZENG W Q, YANG M L, et al. Development and evaluation of a rapid CRISPR-based diagnostic for COVID-19. PLoS Pathogens, 2020, 16(8): e1008705. |
| [42] |
JOUNG J, LADHA A, SAITO M, et al. Point-of-care testing for COVID-19 using SHERLOCK diagnostics. MedRxiv, 2020, 10.1101/2020.05.04.20091231
DOI |
| [43] | 上海交大人投身一线众志成城科技战“疫”, 上海交通大学·新闻学术网, 2020-02-05, https://news.sjtu.edu.cn/jdyw/20200204/119621.html. |
| [44] |
CHEN J S, MA E, HARRINGTON L B, et al. CRISPR-Cas12a target binding unleashes indiscriminate single-stranded DNase activity. Science, 2018, 360(6387): 436.
DOI PMID |
| [45] |
BROUGHTON J P, DENG X D, YU G X, et al. CRISPR-Cas12-based detection of SARS-CoV-2. Nature Biotechnology, 2020, 38(7): 870.
DOI PMID |
| [46] | HOU H Y, WANG T, ZHANG B, et al. Detection of IgM and IgG antibodies in patients with coronavirus disease 2019. Clinical Translational Immunology, 2020, 9(5): 01136. |
| [47] | LIU W B, LIU L, KOU G M, et al. Evaluation of nucleocapsid and spike protein-based enzymeLinked immunosorbent assays for detecting antibodies against SARS-CoV-2. Journal of Clinical Microbiology, 2020, 58(6): 00461. |
| [48] |
AMANAT F, STADLBAUER D, STROHMEIER S, et al. A serological assay to detect SARS-CoV-2 seroconversion in humans. Nature Medicine, 2020, 26(7): 1033.
DOI PMID |
| [49] | 葛均波院士团队联合研发 SARS-CoV-2 IgM 抗体快检试剂盒通过注册检验,新民晚报, 2020-2-18, https://baijiahao.baidu.com/s?id=1658849335805344872&wfr=spider&for=pc. |
| [50] |
DUAN D M, FAN K L, ZHANG D X, et al. Nanozyme-strip for rapid local diagnosis of Ebola. Biosensors and Bioelectronics, 2015, 74: 134.
DOI PMID |
| [51] | WANG H H, LI X M, LI T, et al. The genetic sequence, origin, and diagnosis of SARS-CoV-2. European Journal of Clinical Microbiology & Infectious Diseases, 2020, 39(9): 1629. |
| [52] | ALBERT E, TORRES I, BUENO F, et al. Field evaluation of a rapid antigen test (Panbio COVID-19 Ag rapid test device) for COVID-19 diagnosis in primary healthcare centres. Clinical Microbiology and Infection, 2021, 27(3): 472. |
| [53] |
BARO B, RODO P, OUCHI D, et al. Performance characteristics of five antigen-detecting rapid diagnostic test (Ag-RDT) for SARS-CoV-2 asymptomatic infection: a head-to-head benchmark comparison. Journal of Infection, 2021, 82(6): 269.
DOI PMID |
| [54] |
SEREBRENNIKOVA K V, BYZOVA N A, ZHERDEV A V, et al. Lateral flow immunoassay of SARS-CoV-2 antigen with SERS-based registration: development and comparison with traditional immunoassays. Biosensors, 2021, 11(12): 510.
DOI URL |
| [55] | 国家药监局应急审批2款SARS-CoV-2抗原检测产品广东企业上榜,潇湘晨报, 2020-11-24, https://baijiahao.baidu.com/s?id=1684237376273195168&wfr=spider&for=pc. |
| [56] |
PENG Y S, LIN C L, LONG L, et al. Charge-transfer resonance and electromagnetic enhancement synergistically enabling MXenes with excellent SERS sensitivity for SARS-CoV-2 S protein detection. Nano-Micro Letters, 2021, 13: 52.
DOI PMID |
| [57] |
MORAIS L M C, PARASKEVAIDI M, CUI L, et al. Standardization of complex biologically derived spectrochemical datasets. Nature Protocols, 2019, 14: 1546.
DOI PMID |
| [58] |
YANG L L, YANG Y, MA Y F, et al. Fabrication of semiconductor ZnO nanostructures for versatile SERS application. Nanomaterials (Basel), 2017, 7: 398.
DOI URL |
| [59] |
SHAN Y F, YANG Y, CAO Y Q, et al. Synthesis of wheatear-like ZnO nanoarrays decorated with Ag nanoparticles and its improved SERS performance through hydrogenation. Nanotechnology, 2016, 27(14): 145502.
DOI URL |
| [60] |
YANG Y, NOGAMI M, SHI J L, et al. Self-assembled semiconductor capped metal composite nanoparticles embedded in BaTiO3 thin films for nonlinear optical applications. Journal of Materials Chemistry, 2003, 13(12): 3026.
DOI URL |
| [61] |
YANG L L, PENG Y S, YANG Y, et al. Green and sensitive flexible semiconductor SERS substrates: hydrogenated black TiO2 nanowires. ACS Applied Nano Materials, 2018, 1(9): 4516.
DOI URL |
| [62] |
KIM H, KANG H, KIM H N, et al. Development of 6E3 antibody-mediated SERS immunoassay for drug-resistant influenza virus. Biosensors and Bioelectronics, 2021, 187: 113324.
DOI URL |
| [63] |
WANG C W, WANG C G, WANG X L, et al. Magnetic SERS strip for sensitive and simultaneous detection of respiratory viruses. ACS Applied Materials Interfaces, 2019, 11(21): 19495.
DOI URL |
| [64] |
WANG J F, WU X Z, WANG C W, et al. Facile synthesis of Au-coated magnetic nanoparticles and their application in bacteria detection via a SERS method. ACS Applied Materials Interfaces, 2016, 8(31): 19958.
DOI URL |
| [65] |
WANG C G, LIU M, WANG Z F, et al. Point-of-care diagnostics for infectious diseases: from methods to devices. Nano Today, 2021, 37: 101092.
DOI URL |
| [66] |
PRAMANIK A, GAO Y, PATIBANDLA S, et al. The rapid diagnosis and effective inhibition of coronavirus using spike antibody attached gold nanoparticles. Nanoscale Advances, 2021, 3(6): 1588.
DOI PMID |
| [67] |
ZHANG D Y, ZHANG X L, MA R, et al. Ultra-fast and onsite interrogation of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in waters via surface enhanced Raman scattering (SERS). Water Research, 2021, 200: 117243.
DOI URL |
| [68] |
LIN C L, LIANG S S, PENG Y S, et al. Visualized SERS imaging of single molecule by Ag/black phosphorus nanosheets. Nano-Micro Letters, 2022, 14: 75.
DOI PMID |
| [69] |
ZAVYALOVA E, AMBARTSUMYAN O, ZHDANOV G, et al. SERS-based aptasensor for rapid quantitative detection of SARS-CoV-2. Nanomaterials (Basel), 2021, 11: 1394.
DOI URL |
| [70] |
WU Y X, DANG H J, PARK S G, et al. SERS-PCR assays of SARS-CoV-2 target genes using Au nanoparticles-internalized Au nanodimple substrates. Biosensors and Bioelectronics, 2022, 197: 113736.
DOI URL |
| [71] |
SANCHEZ J E, JARAMILLO S A, SETTLES E, et al. Detection of SARS-CoV-2 and its S and N proteins using surface enhanced Raman spectroscopy. RSC Advances, 2021, 11(41): 25788.
DOI PMID |
| [72] |
LI Y Y, LIN C L, PE Y S. High-sensitivity and point-of-care detection of SARS-CoV-2 from throat and nasal swabs by magnetic SERS biosensor. Sensors and Actuators B: Chemical, 2022, 365: 131974.
DOI URL |
| [73] |
CHEN H, PARK S G, CHOI N, et al. Sensitive detection of SARS-CoV-2 using a SERS-based aptasensor. ACS Sensors, 2021, 6(6): 2378.
DOI PMID |
| [74] |
LEONG S X, LEONG Y X, TAN E X, et al. Noninvasive and point-of-care surface-enhanced Raman scattering (SERS)-based breathalyzer for mass screening of coronavirus disease 2019 (COVID-19) under 5 min. ACS Nano, 2022, 16(2): 2629.
DOI PMID |
| [75] |
PARIA D, KWOK K S, RAJ P, et al. Label-free spectroscopic SARS-CoV-2 detection on versatile nanoimprinted substrates. Nano Letters, 2022, 22(9): 3620.
DOI URL |
| [76] |
LI J R, WUETHRICH A, EDWARDRAJA S, et al. Amplification-free SARS-CoV-2 detection using nanoyeast-scFv and ultrasensitive plasmonic nanobox-integrated nanomixing microassay. Analytical Chemistry, 2021, 93(29): 10251.
DOI PMID |
| [77] |
ZHANG M L, LI X D, PAN J L, et al. Ultrasensitive detection of SARS-CoV-2 spike protein in untreated saliva using SERS-based biosensor. Biosensors and Bioelectronics, 2021, 190: 113421.
DOI URL |
| [78] |
DAOUDI K, RAMACHANDRAN K, ALAWADHI H, et al. Ultra-sensitive and fast optical detection of the spike protein of the SARS-CoV-2 using AgNPs/SiNWs nanohybrid based sensors. Surfaces and Interfaces, 2021, 27: 101454.
DOI URL |
| [79] |
YANG Y, TANEMURA M, HUANG Z R, et al. Aligned gold nanoneedle arrays for surface-enhanced Raman scattering. Nanotechnology, 2010, 21: 325701.
DOI URL |
| [80] |
PENG Y S, LIN C L, LI Y Y, et al. Identifying infectiousness of SARS-CoV-2 by ultra-sensitive SnS2 SERS biosensors with capillary effect. Matter, 2022, 5(2): 694.
DOI URL |
| [81] |
MARQUES A C, PINHEIRO T, MORAIS M, et al. Bottom-up microwave-assisted seed-mediated synthesis of gold nanoparticles onto nanocellulose to boost stability and high performance for SERS applications. Applied Surface Science, 2021, 561: 150060.
DOI URL |
| [82] |
SITJAR J, XU H Z, LIU C Y, et al. Synergistic surface-enhanced Raman scattering effect to distinguish live SARS-CoV-2 S pseudovirus. Analytica Chimica Acta, 2022, 1193: 339406.
DOI URL |
| [83] |
CHEN H, PARK S K, JOUNG Y, et al. SERS-based dual-mode DNA aptasensors for rapid classification of SARS-CoV-2 and influenza A/H1N1 infection. Sensors and Actuators: B. Chemical, 2022, 355: 131324.
DOI URL |
| [84] |
CHEN C, WANG J S. Optical biosensors: an exhaustive and comprehensive review. Analyst, 2020, 145(5): 1605.
DOI PMID |
| [85] |
FIRDOUS S, ANWAR S, RAFYA R. Development of surface plasmon resonance (SPR) biosensors for use in the diagnostics of malignant and infectious diseases. Laser Physics Letters, 2018, 15: 065602.
DOI URL |
| [86] |
LYNN N S, DANDY D S. Passive microfluidic pumping using coupled capillary/evaporation effects. Lab on a Chip, 2009, 9(23): 3422.
DOI PMID |
| [87] |
MARCHESINI G R, KOOPAL K, MEULENBERG E, et al. Spreeta-based biosensor assays for endocrine disruptors. Biosensors and Bioelectronics, 2007, 22: 1908.
DOI URL |
| [88] |
YANO T A, KAJISA T, ONO M, et al. Ultrasensitive detection of SARS-CoV-2 nucleocapsid protein using large gold nanoparticle-enhanced surface plasmon resonance. Scientific Reports, 2022, 12: 1060.
DOI URL |
| [89] |
HUANG L P, DING L F, ZHOU J, et al. One-step rapid quantification of SARS-CoV-2 virus particles via low-cost nanoplasmonic sensors in generic microplate reader and point- of-care device. Biosensors and Bioelectronics, 2021, 171: 112685.
DOI URL |
| [90] |
KAJIURA M, NAKANISHI T, IIDA H, et al. Biosensing by optical waveguide spectroscopy based on localized surface plasmon resonance of gold nanoparticles used as a probe or as a label. Journal of Colloid and Interface Science, 2009, 335(1): 140.
DOI PMID |
| [91] |
PASHCHENKO O, SHELBY T, BANERJEE T, et al. A comparison of optical, electrochemical, magnetic, and colorimetric point-of-care biosensors for infectious disease diagnosis. ACS Infectious Diseases, 2018, 4(8): 1162.
DOI PMID |
| [92] | ZHANG R Q, LIU S L, ZHAO W, et al. A simple point-of-care microfluidic immunomagnetic fluorescence assay for pathogens. Analtical Chemistry, 2013, 85(5): 2645. |
| [93] | TAKEMURA K, ADEGOKE O, SUZUKI T, et al. A localized surface plasmon resonance-amplified immunofluorescence biosensor for ultrasensitive and rapid detection of nonstructural protein 1 of Zika virus. PLoS ONE, 2019, 14(1): 0211517. |
| [94] |
GUERREIRO M R, FREITAS D F, ALVES P M, et al. Detection and quantification of label-free infectious adenovirus using a switch-on cell-based fluorescent biosensor. ACS Sensors, 2019, 4(6): 1654.
DOI PMID |
| [95] |
HUANG R R, HE L, LI S, et al. A simple fluorescence aptasensor for gastric cancer exosome detection based on branched rolling circle amplification. Nanoscale, 2020, 12(4): 2445.
DOI PMID |
| [96] |
WANG Y, LI Z H, WANG J, et al. Graphene and graphene oxide: biofunctionalization and applications in biotechnology. Trends in Biotechnology, 2011, 29(5): 205.
DOI PMID |
| [97] |
SAHA K, AGASTI S S, KIM C, et al. Gold nanoparticles in chemical and biological sensing. Chemical Reviews, 2012, 112(5): 2739.
DOI PMID |
| [98] |
YANG D D, LIU M, XU J, et al. Carbon nanosphere-based fluorescence aptasensor for targeted detection of breast cancer cell MCF-7. Talanta, 2018, 185: 113.
DOI PMID |
| [99] |
LI B M, YU Q L, DUAN Y X. Fluorescent labels in biosensors for pathogen detection. Critical Reviews in Biotechnology, 2015, 35(1): 82.
DOI PMID |
| [100] |
GUO J C, CHEN S Q, TIAN S L, et al. 5G-enabled ultra-sensitive fluorescence sensor for proactive prognosis of COVID-19. Biosensors and Bioelectronics, 2021, 181: 113160.
DOI URL |
| [101] |
ZHOU Y F, CHEN Y, LIU W J, et al. Development of a rapid and sensitive quantum dot nanobead-based double-antigen sandwich lateral flow immunoassay and its clinical performance for the detection of SARS-CoV-2 total antibodies. Sensors and Actuators B: Chemical, 2021, 343: 130139.
DOI URL |
| [102] | CHU Y J, QIU J Y, WANG Y H, et al. Rapid and high-throughput SARS-CoV-2 RNA detection without RNA extraction and amplification by using a microfluidic biochip. Chemistry, 2022, 28: 202104054. |
| [103] |
HAMD-GHADAREH S, HAMAH-AMEEN B A, SALIMI A, et al. Ratiometric enhanced fluorometric determination and imaging of intracellular microRNA-155 by using carbon dots, gold nanoparticles and rhodamine B for signal amplification. Mikrochim Acta, 2019, 186: 469.
DOI URL |
| [104] |
ZHU S J, ZHANG J H, QIAO C Y, et al. Strongly green-photoluminescent graphene quantum dots for bioimaging applications. Chemical Communication, 2011, 47(24): 6858.
DOI URL |
| [105] | NEW S Y, LEE S T, SU X D. DNA-templated silver nanocusters: structural correlation and fluorescence modulation. Nanocale, 2016, 8(41): 17729. |
| [106] |
LIAN J Y, LIU Q, JIN Y, et al. Histone-DNA interation: an effective approach to improve the fluorescence intensity and stability of DNA-templated Cu nanoclusters. Chemical Communication, 2017, 53(93): 12568.
DOI URL |
| [107] |
LIU Y Y, JIANG L P, FAN X J, et al. Intracellular fluorometric determination of microRNA-21 by using a switch-on nanoprobe composed of carbon nanotubes and gold nanoclusters. Mikrochim Acta, 2019, 186: 447.
DOI PMID |
| [108] |
WANG Y H, HE L L, HUANG K J, et al. Recent advances in nanomaterial-based electrochemical and optical sensing platforms for microRNA assays. Analyst, 2019, 144(9): 2849.
DOI URL |
| [109] |
ZHU W Y, SHEN X, ZHU C H, et al. Turn-on fluorescent assay based on purification system via magnetic separation for highly sensitive probing of adenosine. Sensors and Actuators B: Chemical, 2018, 259: 855.
DOI URL |
| [110] |
KUMAR N, HU Y, SINGH S, et al. Emerging biosensor platforms for the assessment of water-borne pathogens. Analyst, 2018, 143(2): 359.
DOI PMID |
| [111] |
ZHANG Z Y, TANG Z M, FAROKHZAD N, et al. Sensitive, rapid, low-cost, and multiplexed COVID-19 monitoring by the wireless telemedicine platform. Matter, 2020, 3(6): 1818.
DOI PMID |
| [112] |
TORRENTE-RODRIGUEZ R M, LUKAS H, TU J, et al. SARS-CoV-2 rapid plex: a graphene-based multiplexed telemedicine platform for rapid and low-cost COVID-19 diagnosis and monitoring. Matter, 2020, 3(6): 1981.
DOI URL |
| [113] |
AKSHATH U S, SHUBHA L R, BHATT P, et al. Quantum dots as optical labels for ultrasensitive detection of polyphenols. Biosensors and Bioelectronics, 2014, 57: 317.
DOI PMID |
| [114] |
NISHITANI S, SAKATA T. Enhancement of signal-to-noise ratio for serotonin detection with well-designed nanofilter-coated potentiometric electrochemical biosensor. ACS Applied Materials Interfaces, 2020, 12(13): 14761.
DOI URL |
| [115] |
DAI Y F, LIU C C. Recent advances on electrochemical biosensing strategies toward universal point-of-care systems. Angewante Chemie International Edition, 2019, 58(36): 12355.
DOI URL |
| [116] |
GOLICHENARI B, NOSRATI R, FAROKHI-FARD A, et al. Electrochemical-based biosensors for detection of Mycobacterium tuberculosis and tuberculosis biomarkers. Critical Reviews in Biotechnology, 2019, 39(8): 1056.
DOI URL |
| [117] |
CHAND R, RAMALINGAM S, NEETHIRAJAN S. A 2D transition-metal dichalcogenide MoS2 based novel nanocomposite and nanocarrier for multiplex miRNA detection. Nanoscale, 2018, 10(17): 8217.
DOI URL |
| [118] |
REICH P, PREUSS J A, BAHNER N, et al. Impedimetric aptamer-based biosensors: principles and techniques. Advances in Biochemical Engineering-Biotechnology, 2020, 174: 17.
DOI PMID |
| [119] | PREUSS J A, REICH P, BAHNER N, et al. Impedimetric aptamer-based biosensors: applications. Advances in Biochemical Engineering- Biotechnology, 2020, 174: 43. |
| [120] |
LOW S S, CHIA J S, TAN M T, et al. A proof of concept: detection of avian influenza H5 gene by a graphene-enhanced electrochemical genosensor. Journal of Nanoscience and Nanotechnology, 2016, 16(3): 2438.
PMID |
| [121] |
MOUSAVI M P S, AINLA A, TAN E K W, et al. Ion sensing with thread-based potentiometric electrodes. Lab on a Chip, 2018, 18(15): 2279.
DOI PMID |
| [122] |
LABIB M, SARGENT E H, KELLEY S O. Electrochemical methods for the analysis of clinically relevant biomolecules. Chemical Reviews, 2016, 116(16): 9001.
DOI PMID |
| [123] | LI Q, LU N, WANG L H, et al. Advances in nanowire transistor-based biosensors. Small Methods, 2018, 2: 1700263. |
| [124] |
BOLLELLA P, GORTON L. Enzyme based amperometric biosensors. Current Opinion in Electrochemistry, 2018, 10: 157.
DOI URL |
| [125] |
CHEN A, CHATTERJEE S. Nanomaterials based electrochemical sensors for biomedical applications. Chemical Society Reviews, 2013, 42(12): 5425.
DOI PMID |
| [126] |
FABIANI L, SAROGLIA M, GALATA G, et al. Magnetic beads combined with carbon black-based screen-printed electrodes for COVID-19: a reliable and miniaturized electrochemical immunosensor for SARS-CoV-2 detection in saliva. Biosensors and Bioelectronics, 2021, 171: 112686.
DOI URL |
| [127] |
EL-SAID W A, AL-BOGAMI A S, ALSHITARI W, et al. Electrochemical microbiosensor for detecting COVID-19 in a patient sample based on gold microcuboids pattern. BioChip Journal, 2021, 15: 287.
DOI URL |
| [128] |
ALAFEEF M, DIGHE K, MOITRA P, et al. Rapid, ultrasensitive, and quantitative detection of SARS-CoV-2 using antisense oligonucleotides directed electrochemical biosensor chip. ACS Nano, 2020, 14(12): 17028.
DOI PMID |
| [129] |
BROSEL-OLIU S, MERGEL O, URIA N, et al. 3D impedimetric sensors as a tool for monitoring bacterial response to antibiotics. Lab on a Chip, 2019, 19(8): 1436.
DOI URL |
| [130] |
ELSHAFEY R, TLILI C, ABULROB A, et al. Label-free impedimetric immunosensor for ultrasensitive detection of cancer marker murine double minute 2 in brain tissue. Biosensors and Bioelectronics, 2013, 39(1): 220.
DOI PMID |
| [131] |
PERSHINA L V, GRABEKLIS A R, ISANKINA L N, et al. Determination of sodium and potassium ions in patients with SARS-CoV-2 disease by ion-selective electrodes based on polyelectrolyte complexes as a pseudo-liquid contact phase. RSC Advances, 2021, 11(57): 36215.
DOI PMID |
| [132] |
TORRES M D T, DE ARAUJO W R, DE LIMA L F, et al. Low-cost biosensor for rapid detection of SARS-CoV-2 at the point of care. Matter, 2021, 4(7): 2403.
DOI URL |
| [133] |
DANIELS J S, POURMAND N. Label-free impedance biosensors: opportunities and challenges. Electroanalysis, 2007, 19(12): 1239.
DOI PMID |
| [134] | AYDIN E B, AYDIN M, SEZGINTURK M K. New impedimetric sandwich immunosensor for ultrasensitive and highly specific detection of spike receptor binding domain protein of SARS-CoV-2. ACS Biomaterials Science Engneering, 2021, 7(8): 3874. |
| [135] |
LORENZEN A L, DOS SANTOS A M, DOS SANTOS L P, et al. PEDOT-AuNPs-based impedimetric immunosensor for the detection of SARS-CoV-2 antibodies. Electrochimica Acta, 2022, 404: 139757.
DOI URL |
| [136] |
PENG Y, PAN Y H, SUN Z W, et al. An electrochemical biosensor for sensitive analysis of the SARS-CoV-2 RNA. Biosensors and Bioelectronics, 2021, 186: 113309.
DOI URL |
| [137] |
KIMMEL D W, LEBLANC G, MESCHIEVITZ M E, et al. Electrochemical sensors and biosensors. Analytical Chemistry, 2012, 84(2): 685.
DOI PMID |
| [138] |
LUO X L, DAVIS J J. Electrical biosensors and the label free detection of protein disease biomarkers. Chemical Society Reviews, 2013, 42(13): 5944.
DOI PMID |
| [139] |
ELDIN N B, EL-RAHMAN M K A, ZAAZAA H E, et al. Microfabricated potentiometric sensor for personalized methacholine challenge tests during the COVID-19 pandemic. Biosensors and Bioelectronics, 2021, 190: 113439.
DOI URL |
| [140] |
CHAIBUN T, PUENPA J, NGAMDEE T, et al. Rapid electrochemical detection of coronavirus SARS-CoV-2. Nature Communication, 2021, 12: 802.
DOI URL |
| [141] |
LEE M Y, LEE H R, PARK C H, et al. Organic transistor-based chemical sensors for wearable bioelectronics. Accounts Chemical Research, 2018, 51(11): 2829.
DOI URL |
| [142] |
MATSUMOTO A, MIYAHARA Y. Current and emerging challenges of field effect transistor based bio-sensing. Nanoscale, 2013, 5(22): 10702.
DOI PMID |
| [143] |
GUTIERREZ-SANZ O, ANDOY N M, FILIPIAK M S, et al. Direct, label-free, and rapid transistor-based immunodetection in whole serum. ACS Sensors, 2017, 2(9): 1278.
DOI URL |
| [144] |
KANG H, WANG X J, GUO M Q, et al. Ultrasensitive detection of SARS-CoV-2 antibody by graphene field-effect transistors. Nano Letters, 2021, 21(19): 7897.
DOI URL |
| [145] |
WANG Z, YI K Y, LIN Q Y, et al. Free radical sensors based on inner-cutting graphene field-effect transistors. Nature Communications, 2019, 10: 1544.
DOI PMID |
| [146] |
GANGULI A, FARAMARZI V, MOSTAFA A, et al. High sensitivity graphene field effect transistor-based detection of DNA amplification. Advanced Functional Materials, 2020, 30: 2001031.
DOI URL |
| [147] |
PICCA R A, MANOLI K, MACCHIA E, et al. Ultimately sensitive organic bioelectronic transistor sensors by materials and device structure design. Advanced Functional Materials, 2019, 30: 1904513.
DOI URL |
| [148] |
SHAO W T, SHURIN M R, WHEELER S E, et al. Rapid detection of SARS-CoV-2 antigens using high-purity semiconducting single-walled carbon nanotube-based field-effect transistors. ACS Applied Materials Interfaces, 2021, 13(8): 10321.
DOI URL |
| [149] |
LI J H, WU D, YU Y, et al. Rapid and unamplified identification of COVID-19 with morpholino-modified graphene field-effect transistor nanosensor. Biosensors and Bioelectronics, 2021, 183: 113206.
DOI URL |
| [150] |
WANG L Q, WANG X J, WU Y G, et al. Rapid and ultrasensitive electromechanical detection of ions, biomolecules and SARS-CoV-2 RNA in unamplified samples. Nature Biomedical Engineering, 2022, 6(3): 276.
DOI PMID |
| [151] |
YOU C C, CHOMPOOSOR A, ROTELLO V M. The biomacromolecule- nanoparticle interface. Nano Today, 2007, 2(3): 34.
DOI URL |
| [152] |
DANIEL M C, ASTRUC D. Gold nanoparticles: assembly, supramolecular chemistry, quantum-size-related properties, and applications toward biology, catalysis, and nanotechnology. Chemical Reviews, 2004, 104: 293.
DOI URL |
| [153] |
BANKS C E, CROSSLEY A, SALTER C, et al. Carbon nanotubes contain metal impurities which are responsible for the “electrocatalysis” seen at some nanotube-modified electrodes. Angewandte Chemie International Edition, 2006, 45(16): 2533.
DOI URL |
| [154] |
SHEN J F, HU Y Z, LI C, et al. Synthesis of amphiphilic graphene nanoplatelets. Small, 2009, 5(1): 82.
DOI PMID |
| [155] |
AYTUR T, FOLEY J, ANWAR M, et al. A novel magnetic bead bioassay platform using a microchip-based sensor for infectious disease diagnosis. Journal of Immunological Methods, 2006, 314: 21.
PMID |
| [156] |
HASH S, MARTINEZ-VIEDMA M P, FUNG F, et al. Nuclear magnetic resonance biosensor for rapid detection of Vibrio parahaemolyticus. Biomedical Journal, 2019, 42(3): 187.
DOI PMID |
| [157] |
SU D Q, WU K, KRISHNA V D, et al. Detection of influenza a virus in swine nasal swab samples with a wash-free magnetic bioassay and a handheld giant magnetoresistance sensing system. Frontiers in Microbiology, 2019, 10: 1077.
DOI PMID |
| [158] |
PASTUCHA M, FARKA Z, LACINA K, et al. Magnetic nanoparticles for smart electrochemical immunoassays: a review on recent developments. Mikrochimica Acta, 2019, 186: 312.
DOI PMID |
| [159] |
SCHOTTER J, KAMP P B, BECKER A, et al. Comparison of a prototype magnetoresistive biosensor to standard fluorescent DNA detection. Biosensors and Bioelectronics, 2004, 19(10): 1149.
PMID |
| [160] |
BAIBICH M N, BROTO J M, FERT A, et al. Giant magnetoresistance of (001)Fe/(001)Cr magnetic superlattices. Physical Review Letters, 1988, 61(21): 2472.
PMID |
| [161] |
BINASCH G, GRUNBERG P, SAURENBACH F, et al. Enhanced magnetoresistance in layered magnetic structures with antiferromagnetic interlayer exchange. Physical Review B: Condensed Matter, 1989, 39(7): 4828.
DOI URL |
| [162] |
BAYIN Q, HUANG L, REN C H, et al. Anti-SARS-CoV-2 IgG and IgM detection with a GMR based LFIA system. Talanta, 2021, 227: 122207.
DOI URL |
| [163] |
ZHANG X J, REEVES D B, PERREARD I M, et al. Molecular sensing with magnetic nanoparticles using magnetic spectroscopy of nanoparticle Brownian motion. Biosensors and Bioelectronics, 2013, 50: 441.
DOI PMID |
| [164] |
ZNOYKO S L, ORLOV A V, BRAGINA V A, et al. Nanomagnetic lateral flow assay for high-precision quantification of diagnostically relevant concentrations of serum TSH. Talanta, 2020, 216: 120961.
DOI URL |
| [165] |
WU K, CHUGH V K, D. KRISHNA V, et al. One-step, wash-free, nanoparticle clustering-based magnetic particle spectroscopy bioassay method for detection of SARS-CoV-2 spike and nucleocapsid proteins in the liquid phase. ACS Applied Materials Interfaces, 2021, 13(37): 44136.
DOI URL |
| [166] |
RÖSCH E L, ZHONG J, LAK A, et al. Point-of-need detection of pathogen-specific nucleic acid targets using magnetic particle spectroscopy. Biosensors and Bioelectronics, 2021, 192: 113536.
DOI URL |
| [167] |
ZALESSKIY S S, DANIELI E, BLUMICH B, et al. Miniaturization of NMR systems: desktop spectrometers, microcoil spectroscopy, and “NMR on a chip” for chemistry, biochemistry, and industry. Chemical Reviews, 2014, 114(11): 5641.
DOI URL |
| [168] |
BEMETZ J, WEGEMANN A, SAATCHI K, et al. Microfluidic- based synthesis of magnetic nanoparticles coupled with miniaturized NMR for online relaxation studies. Analytical Chemistry, 2018, 90(16): 9975.
DOI URL |
| [169] |
LI Y Q, MA P X, TAO Q, et al. Magnetic graphene quantum dots facilitate closed-tube one-step detection of SARS-CoV-2 with ultra-low field NMR relaxometry. Sensors and Actuators B: Chemical, 2021, 337: 129786.
DOI URL |
| [170] |
SCHOENLE M V, LI Y, YUAN M, et al. NMR based SARS-CoV-2 antibody screening. Journal of the American Chemical Society, 2021, 143(21): 7930.
DOI URL |
| [171] |
CANTRELLE F X, BOLL E, BRIER L, et al. NMR spectroscopy of the main protease of SARS-CoV-2 and fragment-based screening identify three protein hotspots and an antiviral fragment. Angewandte Chemie International Edition, 2021, 60(48): 25428.
DOI URL |
| [172] |
NOVAKOVIC M, KUPCE E, SCHERF T, et al. Magnetization transfer to enhance NOE cross-peaks among labile protons: applications to imino-imino sequential walks in SARS-CoV-2-derived RNAs. Angewandte Chemie International Edition, 2021, 60(21): 11884.
DOI URL |
| [173] |
WU K, SAHA R, SU D Q, et al. Magnetic-nanosensor-based virus and pathogen detection strategies before and during COVID-19. ACS Applied Nano Materials, 2020, 3(10): 9560.
DOI URL |
| [174] |
CHOI Y, HWANG J H, LEE S Y. Recent trends in nanomaterials-based colorimetric detection of pathogenic bacteria and viruses. Small Methods, 2018, 2(4): 1700351.
DOI URL |
| [175] | CALVERT A E, BIGGERSTAFF B J, TANNER N A, et al. Rapid colorimetric detection of Zika virus from serum and urine specimens by reverse transcription loop-mediated isothermal amplification (RT-LAMP). PLoS ONE, 2017, 12(9): 0185340. |
| [176] |
ROY S, MOHD-NAIM N F, SAFAVIEH M, et al. Colorimetric nucleic acid detection on paper microchip using loop mediated isothermal amplification and crystal violet dye. ACS Sensors, 2017, 2(11): 1713.
DOI PMID |
| [177] |
WU J J, WANG X Y, WANG Q, et al. Nanomaterials with enzyme-like characteristics (nanozymes): next-generation artificial enzymes (II). Chemical Society Reviews, 2019, 48(4): 1004.
DOI PMID |
| [178] |
WANG Z Q, LI Z S, ZOU Z G. Application of binder-free TiOxN1-x nanogrid film as a high-power supercapacitor electrode. Journal of Power Sources, 2015, 296: 53.
DOI URL |
| [179] |
WANG Z F, YANG X, FENG J, et al. Label-free detection of DNA by combining gated mesoporous silica and catalytic signal amplification of platinum nanoparticles. Analyst, 2014, 139(23): 6088.
DOI PMID |
| [180] | VILELA D, GONZALEZ M C, ESCARPA A. Sensing colorimetric approaches based on gold and silver nanoparticles aggregation: chemical creativity behind the assay. a review. Chemical Society Reviews, 2012, 751: 24. |
| [181] |
ALHOGAIL S, SUAIFAN G, BIKKER F J, et al. Rapid colorimetric detection of pseudomonas aeruginosa in clinical isolates using a magnetic nanoparticle biosensor. ACS Omega, 2019, 4(26): 21684.
DOI URL |
| [182] |
GUO L H, XU Y, FERHAN A R, et al. Oriented gold nanoparticle aggregation for colorimetric sensors with surprisingly high analytical figures of merit. Journal of the American Chemical Society, 2013, 135(33): 12338.
DOI PMID |
| [183] |
ALDEWACHI H, CHALATI T, WOODROOFE M N, et al. Gold nanoparticle-based colorimetric biosensors. Nanoscale, 2017, 10(1): 18.
DOI PMID |
| [184] |
SUN J S, XIANYU Y L, JIANG X Y. Point-of-care biochemical assays using gold nanoparticle-implemented microfluidics. Chemical Society Reviews, 2014, 43(17): 6239.
DOI PMID |
| [185] |
GODAKHINDI V S, KANG P, SERRE M, et al. Tuning the gold nanoparticle colorimetric assay by nanoparticle size, concentration, and size combinations for oligonucleotide detection. ACS Sensors, 2017, 2(11): 1627.
DOI PMID |
| [186] | BÜYÜKSÜNETCI Y T, CITIL B E, TAPAN U, et al. Development and application of a SARS-CoV-2 colorimetric biosensor based on the peroxidase-mimic activity of gamma-Fe2O3 nanoparticles. Mikrochimica Acta, 2021, 188: 335. |
| [187] |
VENTURA B D, CENNAMO M, MINOPOLI A, et al. Colorimetric test for fast detection of SARS-CoV-2 in nasal and throat Swabs. ACS Sensors, 2020, 5(10): 3043.
DOI URL |
| [188] |
GAO Y K, HAN Y K, WANG C, et al. Rapid and sensitive triple-mode detection of causative SARS-CoV-2 virus specific genes through interaction between genes and nanoparticles. Analytica Chimica Acta, 2021, 1154: 338330.
DOI URL |
| [189] |
LEE J K, CHI Y S, S CHOI I. Reactivity of acetylenyl-terminated self-assembled monolayers on gold: triazole formation. Langmuir, 2004, 20: 3844.
PMID |
| [190] |
CHE J, PARK K, GRABOWSKI C A, et al. Preparation of ordered monolayers of polymer grafted nanoparticles: impact of architecture, concentration, and substrate surface energy. Macromolecules, 2016, 49(5): 1834.
DOI URL |
| [191] | KIMLING J, MAIER M, OKENVE B, et al. Turkevich method for gold nanoparticle synthesis revisited. The Journal of Chemical Physics, 2006, 110: 15700. |
| [1] | 朱文杰, 唐璐, 陆继长, 刘江平, 罗永明. 钙钛矿型氧化物催化氧化挥发性有机化合物的研究进展[J]. 无机材料学报, 2025, 40(7): 735-746. |
| [2] | 胡智超, 杨鸿宇, 杨鸿程, 孙成礼, 杨俊, 李恩竹. P-V-L键理论在微波介质陶瓷性能调控中的应用[J]. 无机材料学报, 2025, 40(6): 609-626. |
| [3] | 吴琼, 沈炳林, 张茂华, 姚方周, 邢志鹏, 王轲. 铅基织构压电陶瓷研究进展[J]. 无机材料学报, 2025, 40(6): 563-574. |
| [4] | 张碧辉, 刘小强, 陈湘明. Ruddlesden-Popper结构杂化非常规铁电体的研究进展[J]. 无机材料学报, 2025, 40(6): 587-608. |
| [5] | 吴杰, 杨帅, 王明文, 李景雷, 李纯纯, 李飞. 铅基织构压电陶瓷的发展历程、现状与挑战[J]. 无机材料学报, 2025, 40(6): 575-586. |
| [6] | 姜昆, 李乐天, 郑木鹏, 胡永明, 潘勤学, 吴超峰, 王轲. PZT陶瓷的低温烧结研究进展[J]. 无机材料学报, 2025, 40(6): 627-638. |
| [7] | 陈曦, 袁媛, 谭业强, 刘昌胜. 无机非金属生物材料发展战略研究[J]. 无机材料学报, 2025, 40(5): 449-456. |
| [8] | 田睿智, 兰正义, 殷杰, 郝南京, 陈航榕, 马明. 基于微流控技术的纳米无机生物材料制备: 原理及其研究进展[J]. 无机材料学报, 2025, 40(4): 337-347. |
| [9] | 张继国, 吴田, 赵旭, 杨钒, 夏天, 孙士恩. 钠离子电池正极材料循环稳定性提升策略及产业化进程[J]. 无机材料学报, 2025, 40(4): 348-362. |
| [10] | 殷杰, 耿佳毅, 王康龙, 陈忠明, 刘学建, 黄政仁. SiC陶瓷的3D打印成形与致密化新进展[J]. 无机材料学报, 2025, 40(3): 245-255. |
| [11] | 谌广昌, 段小明, 朱金荣, 龚情, 蔡德龙, 李宇航, 杨东雷, 陈彪, 李新民, 邓旭东, 余瑾, 刘博雅, 何培刚, 贾德昌, 周玉. 直升机特定结构先进陶瓷材料研究进展与应用展望[J]. 无机材料学报, 2025, 40(3): 225-244. |
| [12] | 范晓波, 祖梅, 杨向飞, 宋策, 陈晨, 王子, 罗文华, 程海峰. 质子调控型电化学离子突触研究进展[J]. 无机材料学报, 2025, 40(3): 256-270. |
| [13] | 海热古·吐逊, 郭乐, 丁嘉仪, 周嘉琪, 张学良, 努尔尼沙·阿力甫. 上转换荧光探针辅助的光学成像技术在肿瘤显影中的应用研究进展[J]. 无机材料学报, 2025, 40(2): 145-158. |
| [14] | 孙树娟, 郑南南, 潘昊坤, 马猛, 陈俊, 黄秀兵. 单原子催化剂制备方法的研究进展[J]. 无机材料学报, 2025, 40(2): 113-127. |
| [15] | 陶桂龙, 支国伟, 罗添友, 欧阳佩东, 衣新燕, 李国强. 空腔型薄膜体声波滤波器的关键技术进展[J]. 无机材料学报, 2025, 40(2): 128-144. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||